Older San Franciscans’ fear of becoming a victim of anti-Asian hate may be driving a hidden epidemic of isolation and poorer health, a new UC San Francisco study shows.
What’s new
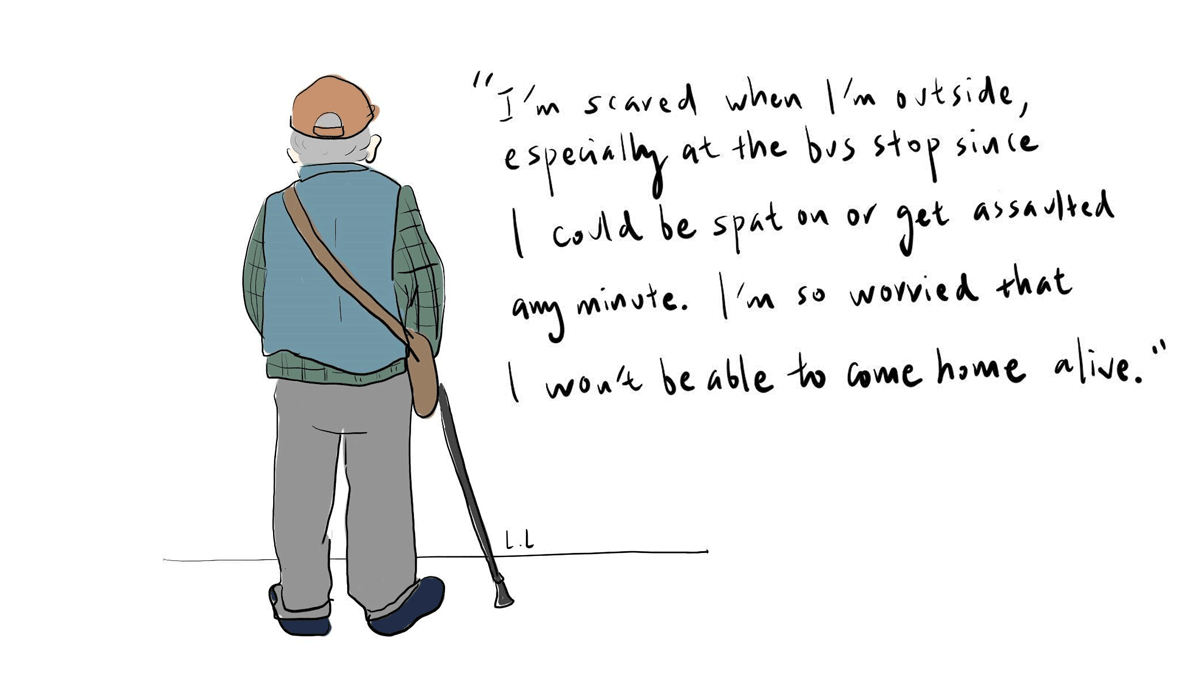
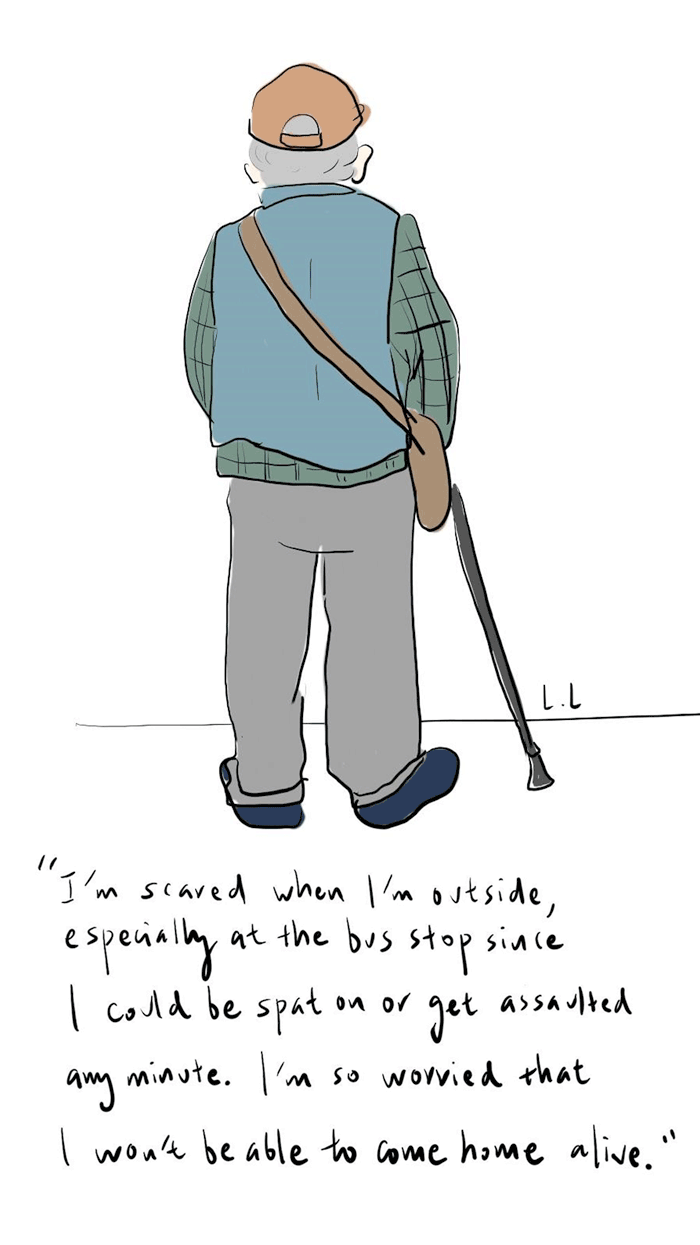
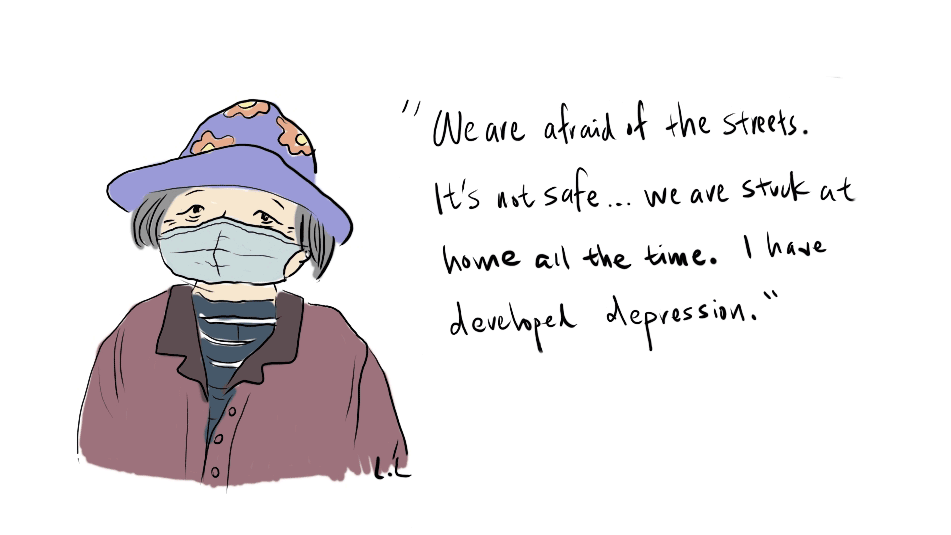
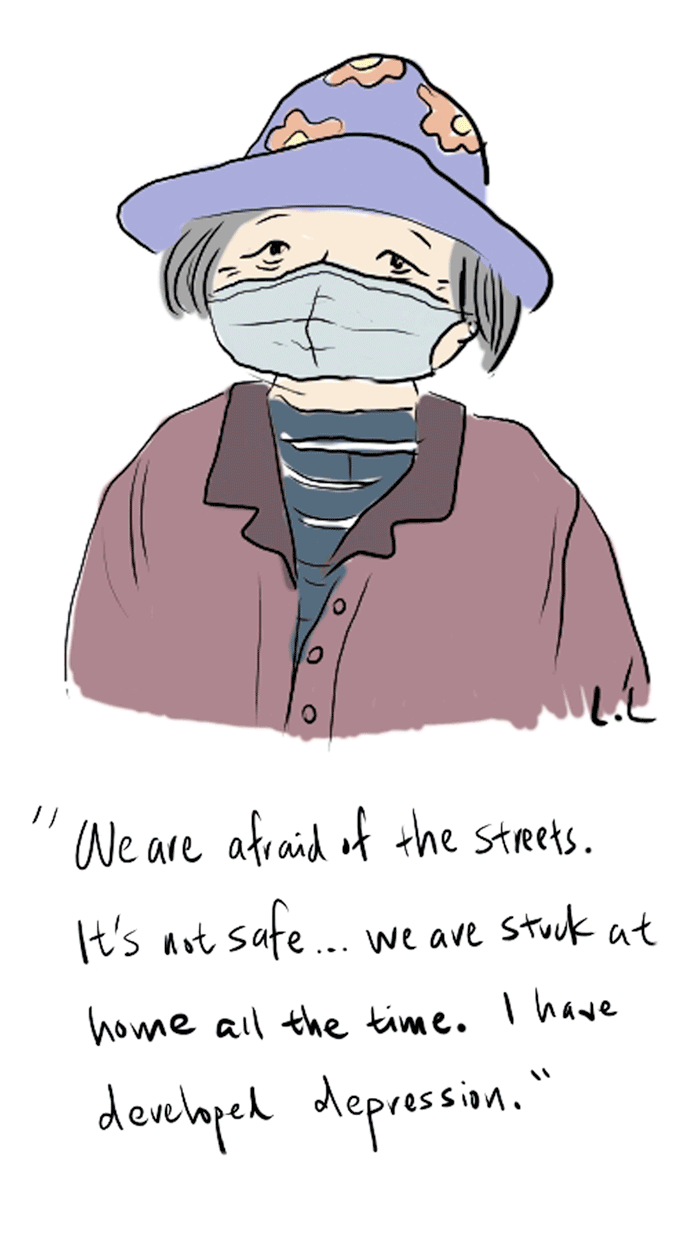
Fearful of becoming a victim of anti-Asian hate, older, Asian San Franciscans are choosing to spend more time at home, forgoing activities that they previously loved, like exercising, seeing loved ones and dining out, suggests the research published as a letter in the journal, JAMA Internal Medicine. This increased isolation may be fueling poorer mental and physical health among the city’s elderly Asian community if results from 80 in-depth interviews among Asian residents 50 years and older and local clinicians are anything to go by.
“We heard a lot of stories about people avoiding going outside to exercise and grocery shop,” explains UCSF Division of Geriatrics fellow Lingsheng Li, MD, MHS. Li carried out the research, alongside a team of UCSF faculty, staff and learners. “Those activities are essential for well-being and quality of life – especially for older adults who are already isolated in the community.”
“Some people even avoided going to the doctor’s office because it required them to get on a bus, which is where many of these attacks have happened.”
The research was supported by the National Institutes of Health.
Among the 20 San Francisco health clinicians interviewed, many reported that isolation exacerbated chronic conditions such as high blood pressure, diabetes and cognitive decline in some patients.
“I’ve seen a few cases where a patient had mild cognitive impairment that worsened to frank dementia,” one physician told UCSF researchers. “After a thorough workup, I have to conclude it’s because they’re no longer going out and walking every day.”
Why it matters
Nationally, 1 in 3 Asians and Pacific Islanders faced racial abuse in 2023. In San Francisco, about a quarter of anti-Asian attacks that targeted Asians 60 years and older between March 2020 and December 2021 involved physical violence.
What does this mean?
Fear of becoming a victim of anti-Asian hate could be a risk factor for poorer mental, social and physical health for older Asian community members. Although some clinicians and patients in Li’s study said they felt screening for this would be difficult, many also felt that addressing racism’s role in health was part of comprehensive health care.
“We also heard very strong recommendations from people who feel like clinicians should screen for anti-Asian hate because it shows clinicians care about the whole person and that acts of racism and violence against them, their families and their communities are not okay,” Li explains. “As clinicians, we may not be able to change the situation right away, but we can still provide that therapeutic listening space and show patients that we care.”
Li’s team co-created a simple screening question with clinicians involved in the study to help start a conversation between patients and health care workers: “Do you feel safe outside of your home?”