As Omicron Surges, UCSF Experts Answer Questions About the COVID-19 Variant
As the holidays approach, new information continues to surface about the Omicron variant of COVID-19. We’ve asked our experts to weigh in on the most common questions we receive about Omicron prevalence, transmission and severity; the safety of holiday gatherings and travel; the new FDA-approved antiviral, and more.
How much Omicron and COVID-19 are we seeing now in the Bay Area and beyond?
Chiu: Omicron is circulating in the Bay Area and is rapidly spreading. We see these same trends – rapidly rising case numbers and proportion of Omicron in California generally and in multiple other states.
Our lab, in collaboration with the San Francisco Department of Public Health and Color Genomics, has found a significant rise in positive tests, with an increasing proportion of Omicron cases. During the first 3 weeks of December, Omicron cases rose from 0 percent of the total positive tests in San Francisco to 68% of the total, while the number of positive cases more than tripled from 38 per week to 128 per week. From December 17 to 20, we had 96 positive samples and 74 (77 percent) of them were Omicron.
CDC data suggest that the proportion of Omicron cases is 90 percent in some parts of the country. This rapid increase is similar to what has been seen across the world. Data from South Africa suggest, however, that Omicron cases may be less severe overall and are less likely to require hospital treatment.
How worried should we be about Omicron?
Gandhi: Omicron is massively more transmissible than delta, perhaps 4 times more. However, there is now evidence that Omicron is less severe than previous strains. We do not know yet if this is because of increasing cellular immunity in the population now or an inherent property of the strain that makes it less virulent, or both.
Two new studies out of the UK and South Africa showed that patients with Omicron were 60 percent to 70 percent less likely to be hospitalized than those with Delta. Other data released from South Africa indicate that average hospital days are shorter than with previous variants (2.8 days compared to eight days); that 90 percent of patients admitted don’t need oxygen therapy with the Omicron variant compared to earlier strains; and that 3% of patients hospitalized recently with COVID-19 have died, versus about 20 percent in the country’s earlier outbreaks.
This reduced severity may be due to increasing immunity in the population or could be partially because the strain is less virulent.
Chin-Hong: South Africa is a younger population, with not as many comorbidities. It has also been recently hit hard by successive waves of natural infection, mostly with Delta. Consequently, there’s a higher population level of immunity (natural plus vaccine) that may not be generalizable to other countries like the U.S. However, this was recently confirmed in studies from England and Scotland showing that omicron infection results in up to two thirds fewer hospitalizations when compared with delta. But the data is evolving. Stay tuned.
What do we know about Omicron and children?
Chin-Hong: We don’t know a lot yet, and what we know mainly comes from South Africa. They saw a lot of kids under age 5 in the hospital with Omicron, but many of them were going in for other reasons. So far, there haven’t been any confirmed deaths of children in South Africa, but they are getting infected because it’s very contagious.
So, children will be protected as long as they can wear a mask and the adults around them are vaccinated. We don’t think outdoors will be that risky; we’re a lot more worried about kids indoors, with all of those mouths and noses close together. We should aim to use the same protocols we did in spring of 2020 – masks, distancing, being outside – to protect ourselves.
Should people be changing their plans for the holidays in light of Omicron?
Chin-Hong: Domestically, I think it’s OK to travel, but you need to up your COVID-safety game. You could double mask or get an N95 mask and make sure it’s tightly fit. If you’re planning on getting together with older members of your family or vulnerable people, you should get tested before that get-together. If you’ll be returning home to immunocompromised or elderly relatives, you’ll want to get a test three or four days after you get back.
What makes the Omicron variant unusual?
Doernberg: This variant’s two most concerning features are: 1) it is very highly contagious and so it is spreading really rapidly, and 2) Omicron is able to get around some of the defenses we have developed over the past couple of years, namely vaccines and monoclonal antibodies.
Information about the severity of infection from Omicron continues to emerge; some reports suggest that severe infections may be less common, but this is a quickly evolving area. Even if this variant proves milder than others, the sheer number of people infected will result in many hospitalizations and will cause many disruptions.
While vaccine effectiveness appears lower for Omicron, the vaccines do still protect against severe disease, and having a booster dose increases the level of protection. Getting vaccinated remains one of the most important defenses. Unfortunately, many of the monoclonal antibodies that we had previously been using for treatment of mild and moderate infections and for post-exposure prevention do not have activity against Omicron. The monoclonal antibody predicted to retain activity, sotrovimab, is in extremely short supply.
What about Omicron’s genetics makes it more transmissible?
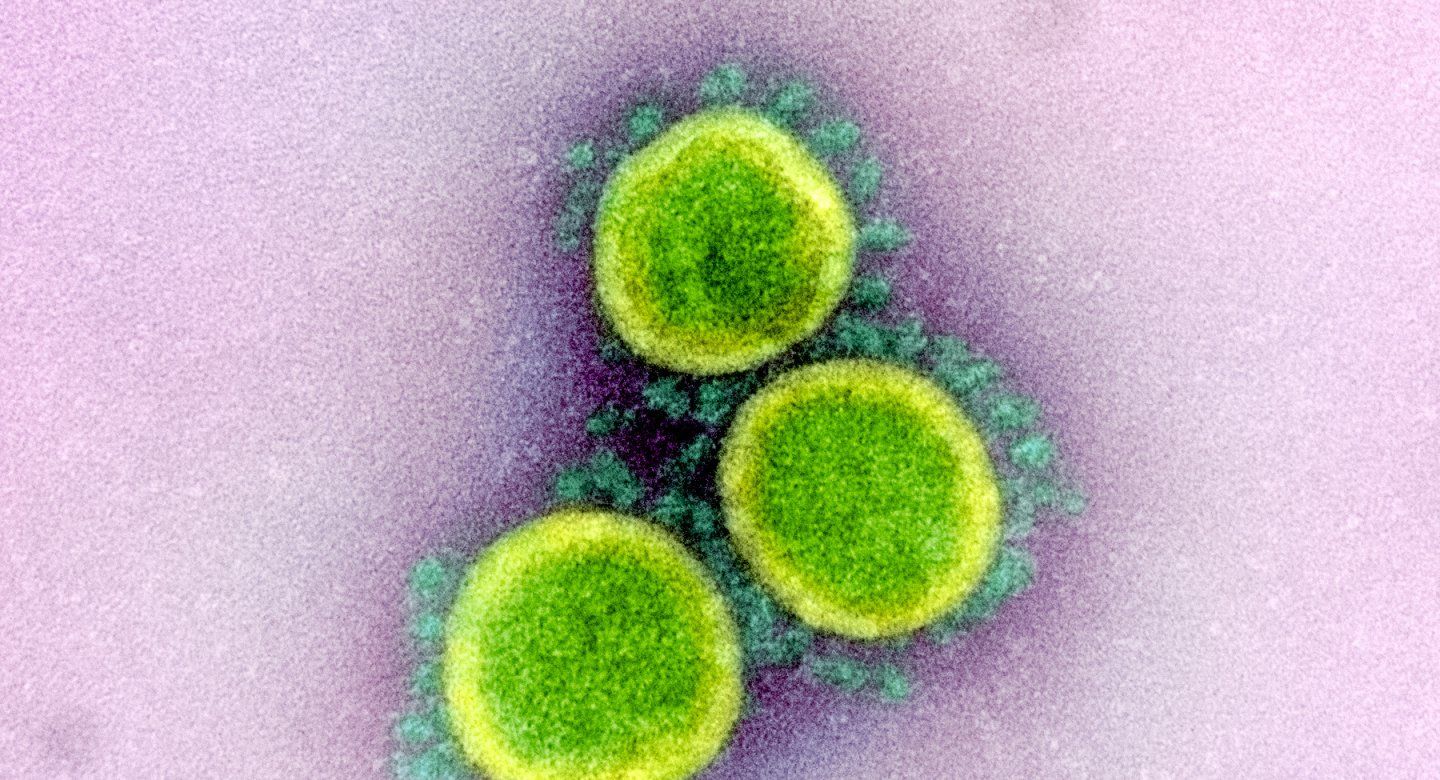
Krogan: Scientists have watched closely as new variants of the virus have amassed mutations in the spike region of the virus's genome, because SARS-CoV-2 uses its spikey outer proteins to get into our cells. Some of these mutations are contributing to increased transmissibility of variants like Alpha, Delta, and now Omicron. The Alpha variant had eight spike mutations; Omicron has more than 30.
But changes are accumulating elsewhere in the virus genome, as well, and it’s important to understand their impact. For this reason, we have been studying mutations outside of spike that could also be contributing to increased transmissibility.
These mutations turn up the expression of certain SARS-CoV-2 proteins that we think help the virus evade the immune response, which could increase the viral load. We’re continuing to study this on a systematic level across all variants to try to understand which mutations make the virus more contagious.
How likely is it with the Omicron variant that people will experience a breakthrough infection if they’ve gotten vaccines and a booster?
Chin-Hong: It’s still possible to get a breakthrough after a booster because this variant looks a little different, but fully vaccinated folks are going can be confident that they’re protected more than most against getting really sick, going to the hospital and dying. I can’t say they won’t get infected, but they’ll have the best chance of anybody of withstanding an infection.
If you’re unvaccinated, you’re going to be very vulnerable to this variant. With two doses of vaccine, you’ll be about 30 percent protected. Boosted, it will be about 80 percent protection.
One relatively small study found that if you have a breakthrough case and both vaccine doses, your immune level goes through the roof. You have 1,000 times the antibodies compared to people two weeks after their second dose.
And if you’re boosted and get an infection, the chances of you withstanding a future variant is the highest on the planet. If you’re walking on the street, COVID will probably be running away from you.
What do we know about vaccines, boosters and long COVID?
Rutherford: We don’t know anything about long COVID among people who are vaccinated and boosted, but we expect that it will be a lot less common.
Why is it so hard to get boosters? Is there a shortage?
Rutherford: There is a mismatch between supply and demand for boosters. In some areas, like San Francisco, demand is high but the number of people available to give the vaccines is insufficient. In other parts of California, there is a sufficient supply of boosters and people to give them, but the demand has not yet increased to match the available supply. The bottom line is that in some places, you’re going to have to work to get a booster (lots of calls, etc.) while in others it will be easy.
The FDA just approved Pfizer’s antiviral pill, Paxlovid, to treat COVID-19 in high-risk individuals who are at least 12 years old and weigh at least 88 pounds. What impact will this antiviral have?
Doernberg: I think the drug has really great promise for patients at high risk for complications from COVID, like those with medical comorbidities. There will be some barriers as we are getting off the ground. One is that the drug was shown to be effective within five days of symptoms and ideally should be taken within three days of symptoms. It can be hard to get a COVID test and a result in five days, especially in times when there are surges.
The other thing is that the drug will be in short supply initially; it won’t be available at first to every patient. Also, it will likely take several days before the drug is allocated and delivered to pharmacies. Medical systems will need to build out their electronic medical records so they can prescribe it. There are some drug interactions to consider, as some of the patients who are at highest risk of COVID, like transplant patients, are also on medications that would have a bad interaction with the antiviral – so that adds complexity in terms of prescribing it.
Are we headed for further restrictions?
Rutherford: I think it’s quite possible. In California, for instance, a mask restriction has been put into effect for one month through mid-January. I don’t think we’ll be seeing business closures again. Some businesses are having trouble getting workers, so that may have an impact, but I don’t see us returning to widespread shelter-in-place orders.