A new study, led by UC San Francisco, reveals that quality of sleep, not quantity, may play a part in the development of dementia decades before symptoms start.
Unlike previous research that has primarily focused on sleep disturbance and cognitive impairment in late life, the 526 participants at the start of this study had an average age of 40.
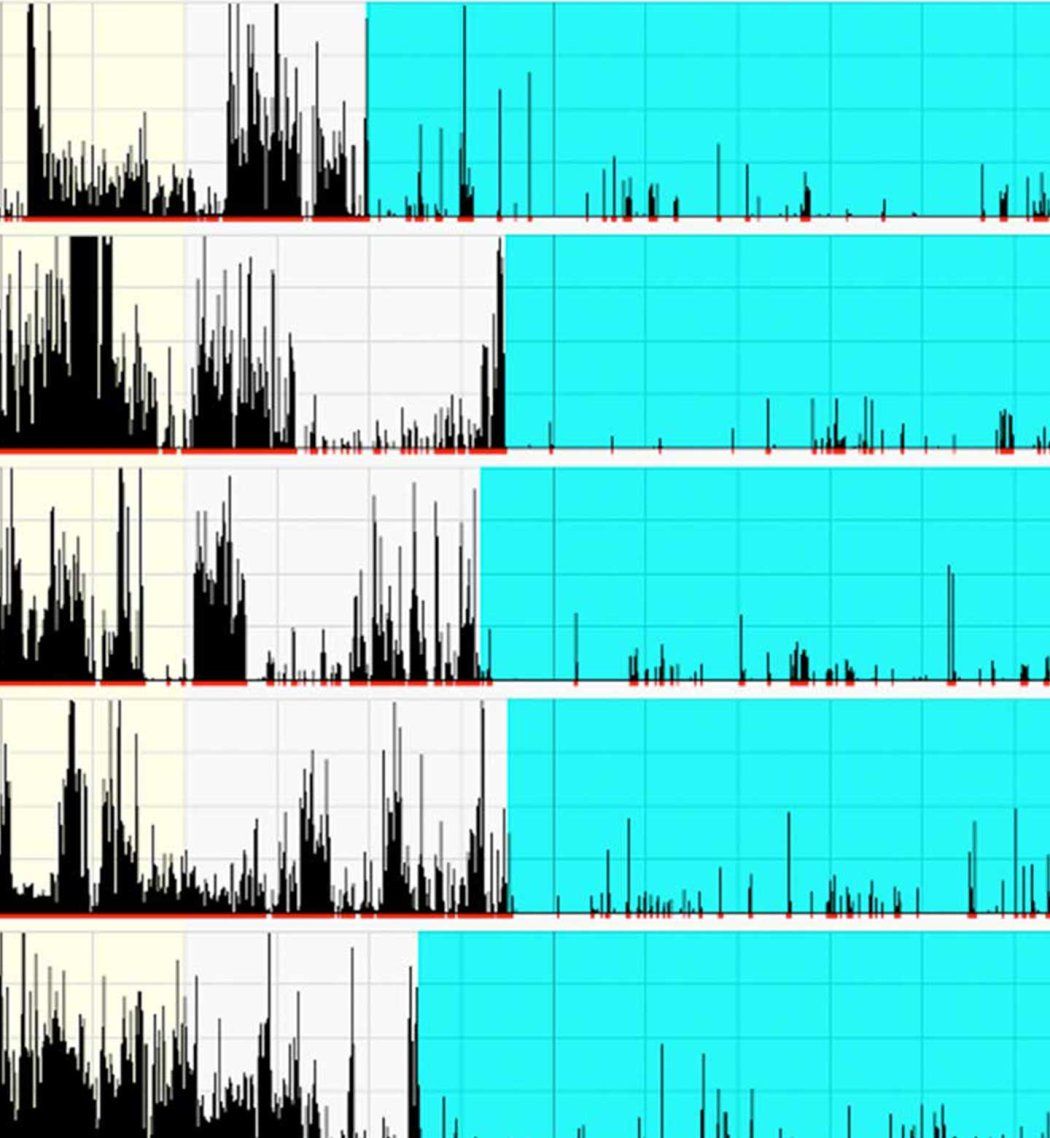
And while most earlier studies have relied on subjective measures of sleep quality, the researchers used a wrist activity monitor to record bedtime “sleep fragmentation,” which took into account the amount of time participants were immobile and the amount of time they were moving.
The study, publishes in the journal Neurology on Jan. 3, 2024.
After tracking the participants’ sleep habits and evaluating their cognitive performance years later, the researchers found no association between cognition and sleep duration, in analyzing both self-reports and data from the wrist activity monitors.
In contrast, those with higher levels of fragmented sleep were found to be up to three times as likely to score below average in cognitive testing as those with lower levels of fragmented sleep, when adjusted for factors like education, depression, body mass index, diabetes and hypertension.
“Since Alzheimer’s disease pathology begins to accumulate in the brain many years before symptoms onset, it’s possible that sleep disturbances identified in late life – close to the time when memory loss becomes apparent – is actually the consequence of this pathology that has been developing silently over the years,” said first author Yue Leng, PhD, of the UCSF Department of Psychiatry and Behavioral Sciences, and the Weill Institute for Neurosciences.
“Given the long, symptom-free window of Alzheimer’s disease and the high prevalence of sleep problems, the understanding of midlife sleep disturbances has significant public health implications.”
Currently 1 in 9 Americans aged 65 and older suffer from Alzheimer’s. However, recent studies show that up to 40% of cases may be prevented or delayed by making health changes, including practicing good sleep hygiene.
A toll on executive function
The participants were part of CARDIA (Coronary Artery Risk Development In young Adults), a National Institutes of Health study. Over half were female; 56% were white and the remainder were Black. Their sleep habits were assessed over a three day-period on two occasions, approximately one year apart, and cognitive testing took place about 11 years later.
The researchers divided the participants’ sleep quality scores into three groups: those with higher, moderate and lower levels of sleep fragmentation. Participants in the higher group were 2.10 to 2.97 times more likely to score below average on four tests measuring executive function, as well as working memory, processing speed and global cognition, compared to those in the lower group.
Surprisingly, a fifth test, quantifying verbal memory, did not show differences between these two groups.
“This confirms previous studies of older adults suggesting a strong association between sleep disorders and executive function, which might be due to the influence of sleep on the prefrontal cortex area, the seat of executive function, rather than verbal memory,” Leng said.
No difference was found in cognitive scores between those with moderate sleep fragmentation compared with lower sleep fragmentation. Cognitive performance and sleep fragmentation did not differ by race or sex. There was no association between cognition and sleep quality when it was measured subjectively.
“This research contributes to a body of literature that underscores the need to evaluate modifiable risk factors associated with cognitive aging,” said senior author Kristine Yaffe, MD, of the UCSF departments of Psychiatry and Behavioral Sciences, Neurology, and Epidemiology and Biostatistics.
“Future research is needed to study the link between sleep disturbances and cognition at different stages of life and to identify whether there are critical life periods when sleep is more strongly associated with cognition,” added Yaffe, who is a member of the first team of experts to determine that 30% of dementia risk is preventable. “This might open up new opportunities for the prevention of Alzheimer’s in late life.”
Co-Authors: Kristen Knutson, PhD, of UCSF and Mercedes R. Carnethon, PhD, of Northwestern University.
Funding: The CARDIA study is supported by contracts HHSN268201800003I, HHSN268201800004I, HHSN268 201800005I, HHSN268201800006I and HHSN268201800007I from the National Heart, Lung, and Blood Institute (NHLBI). The CARDIA Cognitive Function ancillary study is supported by NHLBI grant R01 HL122658. The authors report no relevant disclosures.