Malaya was wearing a tank top on a warm day in December 2020 when her parents noticed her right shoulder blade protruding in an unusual way. Concerned, they saw her pediatrician the next day who ordered an X-ray. Her mother, Mary, was standing beside the X-ray technician, and her heart dropped when the X-ray appeared on the screen. It was clear, even to her untrained eyes, that Malaya’s spine had a severe s-curve.
Overnight, Malaya went from being a healthy 13-year-old who’d just had a big growth spurt to a scoliosis patient. Her family turned to UCSF Benioff Children’s Hospital Oakland for an innovative solution that uses 3D imaging during surgery.
Instead of having a straight spine, scoliosis patients have s-shaped or c-shaped curves in their spines that may cause their shoulders or hips to be uneven. There are about 6 million scoliosis cases in the United States, up to about 4% of the population, according to the Scoliosis Research Society. It mostly affects adolescents, and girls are 10 times more likely to have scoliosis than boys.

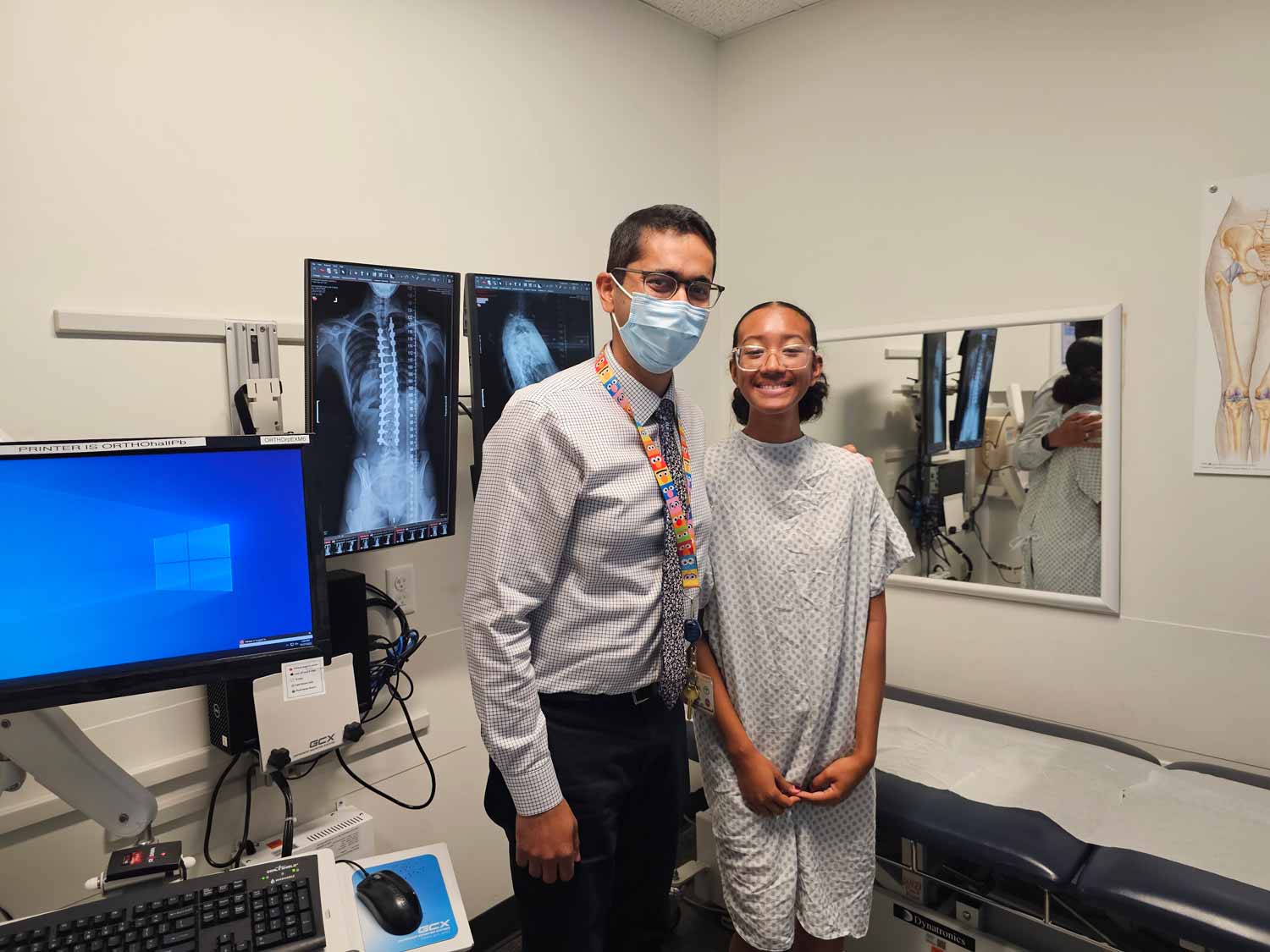
Malaya tried treating her scoliosis with a back brace, but over the next year, her curve got worse. She was referred to Ishaan Swarup, MD, a pediatric orthopedic surgeon at UCSF Benioff Oakland, who said that given the magnitude of her curve, she needed surgery. Without it, her scoliosis curve would get more severe as she continued growing and could start causing pain and mobility issues.
“We were nervous before the surgery, but we trusted Dr. Swarup and were confident he and his team would do a great job,” said Mary. An athletic and energetic teenager, Malaya was eager to “get fixed” before she had pain and wanted to return to school sports, like ultimate frisbee, and family activities like zip lining, hiking and white-water rafting.
A new level of precision surgery
During an eight-hour surgery in August 2022, Swarup placed two rods and 26 screws in Malaya’s spine using special intraoperative 3D CT scanner technology, called a Medtronic O-arm. The O-arm was positioned like a ring around Malaya and scanned her body as she lay on the operating table, providing Swarup with views of her exact anatomy in real-time on large, high-definition screens.
The benefits of using the 3D CT scanner are more precise screw placements, shorter surgeries, less anesthesia, less removal of soft tissue and less blood loss. Patients recover faster and easier and require fewer follow-up surgeries to adjust the placement of hardware, Swarup explained.
X-rays are a common imaging tool used by surgeons in advance of and during surgeries, but they only provide two-dimensional images. CT scans create three-dimensional images of internal anatomy.
“In a traditional spinal fusion surgery, we’d find and use anatomical landmarks when placing hardware. But with scoliosis and other situations, the anatomy is altered for most patients, which makes it more challenging to place screws and rods,” said Swarup, who is the director of UCSF’s Pediatric Orthopedic Trauma department and specializes in scoliosis and other spinal disorders, hip conditions and traumatic injuries.
“Now, using the 3D CT scans during our spinal operations we can see in a whole new way,” he added. “We can visualize a cross-section or change angles, make measurements, even recreate the spine on the screen so we can place the hardware with a new level of safety, precision and accuracy.”
Since purchasing two 3D CT scanners two years ago, Swarup and his colleagues have used them on all their pediatric spinal surgeries at UCSF Benioff Oakland, and many surgeries at the San Francisco campus. More than 50 patients have benefited so far, and the numbers are growing. It’s most frequently used to treat different types of scoliosis and spina bifida, as well as traumas – since UCSF Benioff Oakland is the only pediatric Level 1 Trauma Center in the East Bay.
The technology is also used as a teaching tool, explained Swarup. “As a teaching institution, we’re teaching the surgeons of tomorrow. These 3D CT scanners allow me to display the anatomy and scoliosis pathology to the residents and fellows, so they get a better understanding of the condition and how we safely take care of it. It helps them learn to become independent practitioners in the future.”
Back in action
Malaya’s surgery successfully returned her spine to a straighter position, and she and her family are pleased at how easy her recovery was. She was able to stop using pain medication just days after the surgery. A month later, she returned to her high school in San Leandro. She’s been in physical therapy this year to increase her strength and flexibility.
“Dr. Swarup has magic hands,” said Mary, who’s grateful that their life is returning to normal. “The whole UCSF team was so helpful throughout the process, making it smooth and easy – from the surgery to disability paperwork for Malaya’s school. And now Malaya has started running, walking and swimming again.”
“I’ve really accomplished something and overcome a big challenge in my life,” Malaya said.
“I now know that I can keep pushing and do so much. I just got the all-clear to try out for sports teams at school, and I can’t wait for ultimate frisbee tryouts!”