Brain Stimulation for Stroke Recovery, Brain Implants for Speech Among Conference Talks
UCSF Experts to Highlight Cutting Edge Advances and Discoveries at World’s Largest Meeting Devoted to Neuroscience
Brain implants for speech, neurological effects of COVID-19, and motor recovery after stroke are among the topics that researchers from UC San Francisco (UCSF) will be presenting at this year’s annual meeting of the Society for Neuroscience.
The conference, happening November 12-16 in San Diego, is the world’s largest gathering devoted to neuroscience, bringing together over 20,000 researchers, clinicians, and advocates. This year’s attendees can choose to be in person or online.
Here are some highlights of research being presented by UCSF faculty:
Neurotechnology
Press conference: Sunday, Nov. 13, 1:00 pm
(in-person and virtual)
UCSF is a world leader in research into the use of implanted brain devices and AI to address an array of conditions. In this press conference, graduate student Sean Metzger will discuss his work with Edward Chang, MD, and a study participant who became severely paralyzed after a car accident and stroke. Previously, the lab created a “neuroprosthesis” that allowed the participant to communicate by attempting speech. In their most recent study, the team successfully enabled the participant to spell out letters by attempting to say them.
On Nov. 16, the work of anesthesiologist Prasad Shirvalkar, MD, PhD, who is conducting a clinical trial using personalized deep brain stimulation (DBS) to treat chronic pain, will be highlighted in two poster presentations.
Neurological Consequences of COVID-19
In a symposium on Sat., Nov. 12, neurologist Joanna Helmuth, MD, MHS, of UCSF’s Memory and Aging Center, and infectious disease specialist Michael Peluso, MD, one of the leaders of UCSF’s Long-term Impact of Infection with Novel Coronavirus (LIINC) study, will discuss their findings of biomarkers in cerebral spinal fluid and plasma of patients with neurological long COVID symptoms.
In the LIINC study, Peluso has found markers of inflammation as well as viral particles and metabolic changes in brain cells from patients with long COVID. Studying a subset of 13 long COVID patients, Hellmuth found abnormalities in their cerebral spinal fluid as well.
Stroke Recovery
On Tues., Nov. 15, postdoctoral researchers working with neurologist Karunesh Ganguly, MD, PhD, who has long worked to develop implantable neurotechnology to help stroke patients, will discuss their latest research into how parts of the brain that govern manual dexterity change during recovery after being damaged in a stroke. Ian Heimbuch, PhD, and Preeya Khanna, PhD, will discuss how brain areas devoted to movement control and sensation change after stroke and change again during recovery, communicating with each other in different ways.
In a third talk, Hoseok Choi, PhD, will describe how he used targeted brain stimulation in mice to restore communication between areas and improve brain function. Understanding how brain areas communicate is critical to moving forward with studies in humans, Ganguly said, and he is optimistic that brain stimulation will become more reliable and customizable for patients.
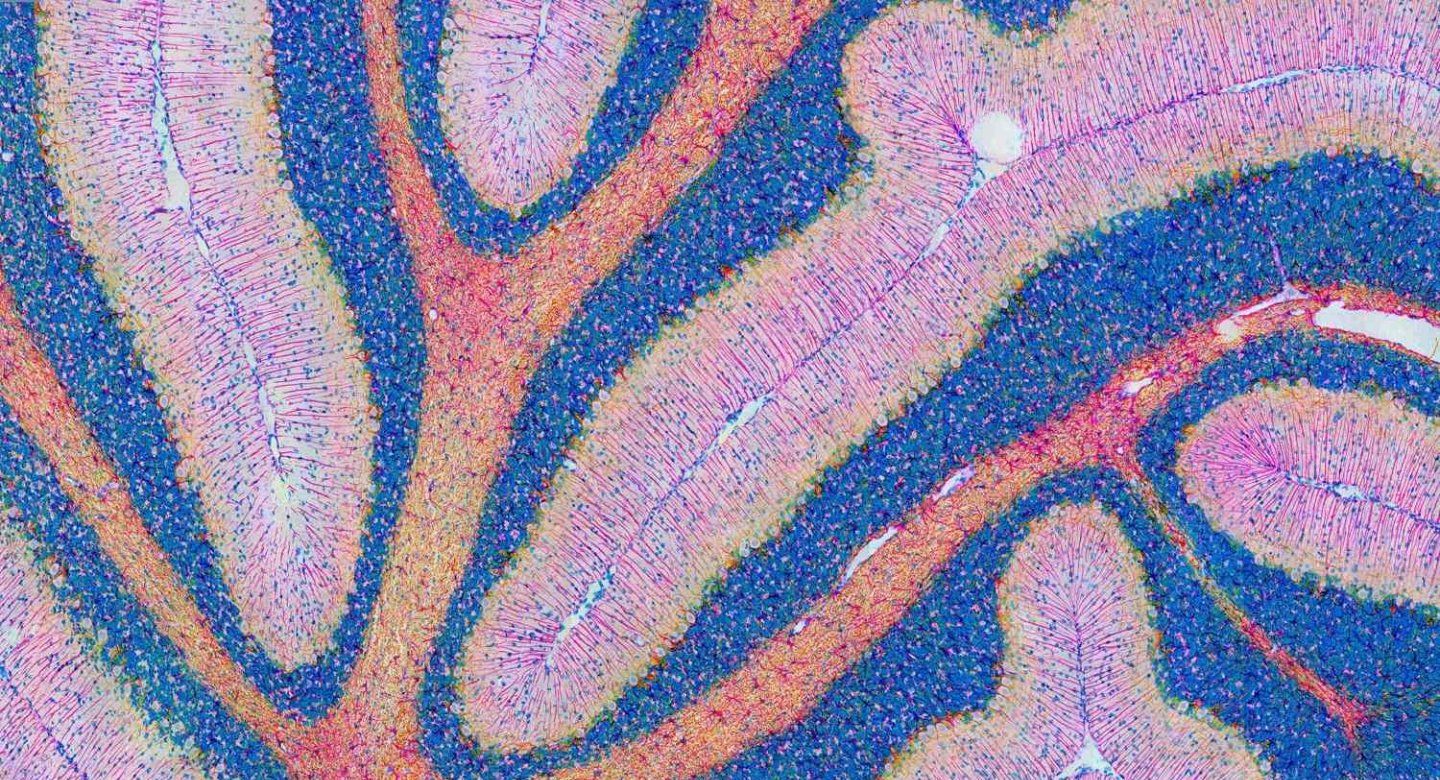
Astrocytes
While neurons get most of the attention in neuroscience, the human brain’s most numerous cells, called astrocytes, are garnering increasing interest as it becomes clear that these “support cells” have multiple, previously unappreciated roles. Indigo Rose, MS, a PhD student in the lab of cell biologist Martin Kampmann, PhD, will present his work investigating how, in models of brain disease, these cells produce toxic lipids that may kill neurons. Understanding how this neurotoxic process works could lend a new view of how neurodegenerative diseases operate.
In another presentation from the Kampmann lab, PhD student Emmy Li, BA, will discuss her work with iAssembloids, three dimensional cultures made up of neurons, astrocytes, and microglia (cells that act as the brain’s immune system) to look at the effects of erratic neuronal activity commonly associated with seizures, and which can accompany neurodegenerative diseases. She found that these bursts of excessive stimulation may produce reactive oxygen molecules that set off a neurodegenerative process, and that altering a key pathway related to a protein called GSK3B can be protective against this process.