Viruses Mutate, But Treatments Are Static. Is There a Way to Change That?
There is a big, global problem: viruses such as HIV and COVID-19 mutate, but treatments for them don’t.
For more than 20 years, Leor Weinberger, PhD, has been thinking about how to make vaccines work more efficiently by being adaptive, rather than static.
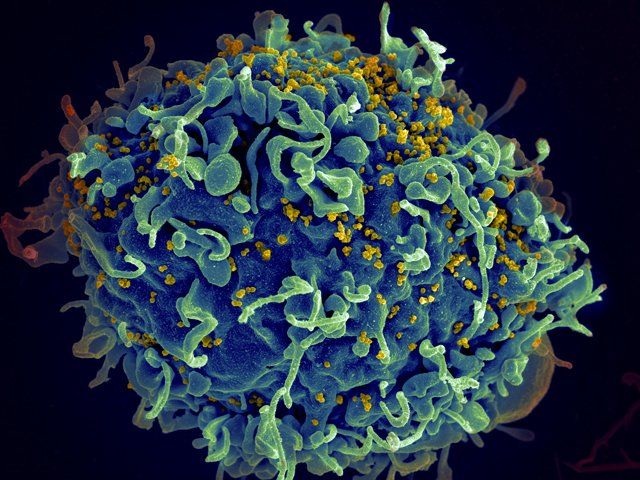
A human T cell (blue) is under attack by HIV (yellow), the virus that causes AIDS. Image by NIH
“We’re fighting biology with chemistry,” said Weinberger, director of the Gladstone Center for Cell Circuitry and a professor in the Departments of Pharmaceutical Chemistry and Biochemistry and Biophysics at UC San Francisco. “Biology is dynamic, so it evolves. It transmits. Chemistry does neither of those things. It’s static.”
Up until last year, Weinberger’s work primarily focused on HIV, a virus that continues to infect nearly 2 million people a year worldwide, despite anti-retroviral treatments. He praises these drugs as “a miracle of modern medicine,” and they work well in individuals, but don’t have success on a population scale because they need to be taken daily, for life. So-called super spreaders, the 20 percent of the population that drives 80 percent of infections, can also be hard to reach as often they’re maligned and stigmatized sex workers or injection drug users. They’re less likely to have access to these life-saving drugs, and even if they did, those treatments don’t prevent infections from taking hold.
The antivirals mostly are defensive – taken once a person is infected by the virus. Efforts to create a vaccine for HIV have been elusive since the virus mutates rapidly. Though slower in its rate, COVID-19 can also mutate, which already is making vaccines less effective against some strains, and why as the virus continues to evolve, it holds the potential to escape current vaccines entirely.
For Weinberger, the William and Ute Bowes Distinguished Professor, the idea is to avoid fighting viruses from a defensive position. He has developed Therapeutic Interfering Particles (TIPs) that go on offense. They do this by “hijacking the hijackers,” he said.
Hijacking Replicating Material
Viruses proliferate because they infect cells, use those cell’s resources to create more of themselves, and then go forth and infect more cells, over and over and over again, spreading inside one’s own body until there is enough virus in the body to infect other people.
TIPs are engineered mutants of the virus themselves, little snippets of similar DNA. They outcompete the virus for replicating material, so instead of spreading the virus, the virus spreads the harmless mutant. As the TIPs spread, the virus fails to replicate further, decreasing the viral load.
While TIPs aren’t antivirals, they also are different than vaccines. “Vaccines present part of the virus to the immune system and trains it to fight a live infection if it ever comes across one,” he said. “TIPS work by interfering with different components of the virus.”
While TIPs are effective in stopping viral spread inside one person, they can also help bring a pandemic to heel through the same super-spreaders that push on a pandemic. Instead of super spreading the virus, they super spread the TIPs. Because the TIP is inherently the virus it combats, it can evolve in the same way alongside the virus.
20 Years, Thousands of Dead Ends
Weinberger started thinking of dynamic virus solutions while in graduate school at UC Berkeley, and has faced an uphill battle along the way. It took 20 years and more than 150,000 dead ends until his lab found a TIP that worked – almost by accident.
We’re fighting biology with chemistry Biology is dynamic, so it evolves. It transmits. Chemistry does neither of those things. It’s static.
A mutant that had formed on its own in a viroreactor running in the back of the laboratory – which Weinberger stresses is not a euphemism. The reactor really was sitting in the back on a shelf, waiting for them to find a TIP that worked. Elizabeth Tanner, PhD, a postdoctoral student, checked to see if anything interesting was happening inside and found the first successful TIP had formed on its own.
After testing the TIP in animal models, Weinberger is preparing his first clinical trial for later this year, which will be done with HIV positive patients who also have a terminal illness.
Weinberger says he’s faced resistance to this kind of technology, even though it’s not new. Albert Sabin’s oral polio vaccine, which became the predominant polio vaccine in the 1960s onward, also broke the chain of transmission in a similar fashion, though he said that property of the vaccine is not well known.
Overall, Weinberger said, the U.S. scientific community is less comfortable talking about anything that feels like genetic engineering, especially changes that can be passed onto other people. There is more enthusiasm for this type of solution in Africa, where nearly 20 million people have HIV, and where in 2019, about 150,000 children contracted the virus.
A Pivot to COVID-19
In March 2020, Weinberger presented his research at TedMed 2020, a talk that one of the organizers of TED said received the “most enthusiastic and complete standing ovation" in his memory. The Boston event was one of the last major gatherings to be held before the COVID-19 pandemic made such in-person gatherings dangerous.
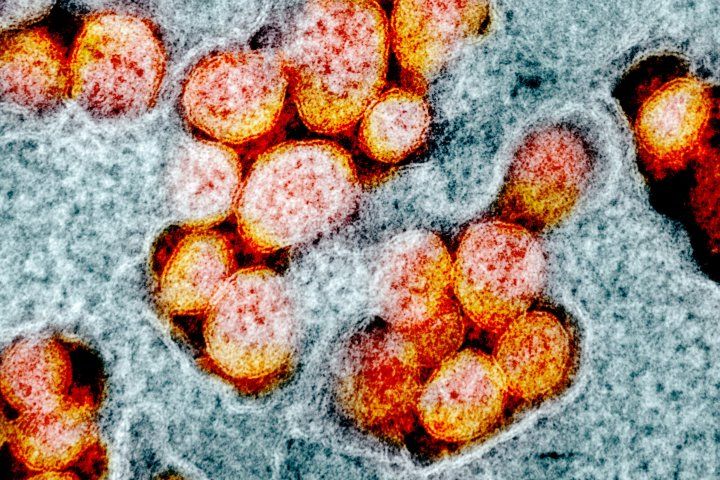
Leor Weinberger, PhD, has pivoted his work from HIV to COVID-19 in the past year. Image by NIH
His lab has since pivoted to applying TIP technology to creating new therapeutics for COVID-19. In July, the Weinberger Lab received a grant, in partnership with VxBiosciences Inc., to study how TIPs could be used in the global effort to control COVID-19.
“Mutants are going to arise and we’re going to have trouble distributing the vaccine,” Weinberger said. TIPS can be “another tool that might be able to back burn some of the pandemic strains that come up.”
While vaccines are the front-line defense, they are still static, bringing him back to his original quandary from more than 20 years ago.
“We can make vaccines fairly quickly. That’s not the problem,” he said. “The problem is distributing them and remaking them – where with TIPs, they take care of that on their own.”