Flipping A Genetic Switch on Cells Lets Researchers Boost or Suppress Immune Responses
Research Points Toward Immunotherapies for Cancer and Autoimmune Diseases
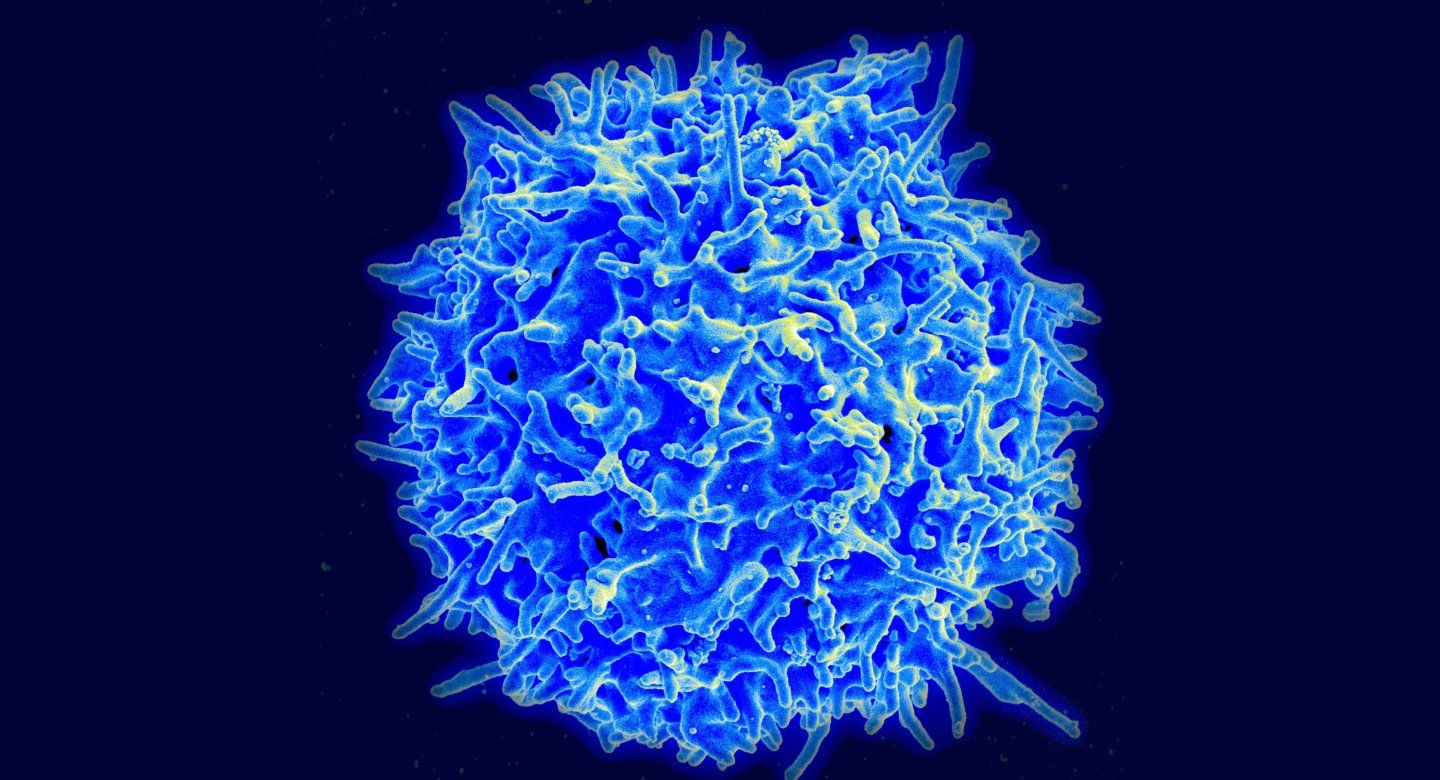
Cancer and autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis, might not seem to have much in common, but some researchers now are pinning hopes on the same immune system cell – called the regulatory T cell, or Treg – to better fight both, through immunotherapies that manipulate these cells in opposing ways to fight the two disease types.
A key role of Tregs is to dampen the destructiveness of another type of T cell, called an effector T cell, a warrior cell that actively targets invading pathogens and tumors. By calming T effectors, Tregs help the immune system return to a normal level of guardedness after a vigorous battle against infection has been won.
Autoimmune disease has been linked to weak Treg responses that fail to fully restrain effector T cells, allowing them to attack the body’s own tissues. In contrast, in many common types of tumors, high levels of suppressive Tregs in the vicinity of the cancer can prevent the immune system from attacking the tumor, which has been linked to worse outcomes.
In a new study published on April 29, 2020, in Nature, UC San Francisco and Northwestern University scientists identified genes with the potential to be manipulated clinically as a kind of switch for Tregs. Flipped one way by perturbation of a gene, the switch can drive Tregs to allow the immune system to more vigorously attack rogue cancer cells within the body. Flipped the opposite way, by perturbing a different gene, the switch may keep the immune system from attacking the body’s own tissues in autoimmune diseases.
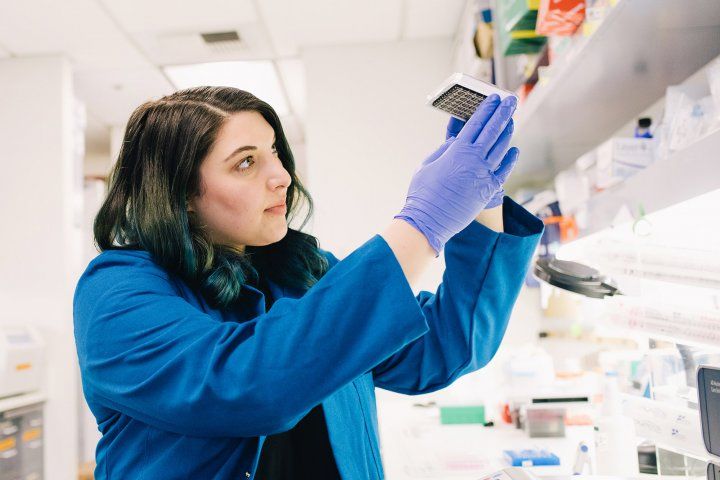
Jessica Cortez
“Tregs exerting their normal suppressive function can prevent your immune system from fully tackling cancer, but we found a way to flip a switch to dampen that suppression resulting in an enhanced anti-tumor immune response,” explained UCSF graduate student Jessica Cortez, a lead author of the new study, who conducted many of the experiments in the lab of senior co-author Alexander Marson, MD, PhD, a UCSF immunologist.
“This study demonstrates a promising approach to manipulate Tregs that eventually could help to boost the immune response for cancer treatments or rein it in for autoimmune disease treatments,” said Marson, an associate professor of microbiology and immunology at UCSF, CZ Biohub investigator, and scientific director for biomedicine at the Innovative Genomics Institute, a joint research collaboration between UCSF and UC Berkeley focused on CRISPR.
To identify their Treg-switching modulators, Cortez and colleagues inserted genetic instructions to prevent Tregs from producing one of 489 selected regulatory proteins normally found in Tregs and/or T effector cells, using CRISPR-based gene-targeting technology.

Alex Marson, MD, PhD
A winner that emerged from screening was a protein called ubiquitin specific peptidase 22 (Usp22), which, when absent, diminished Treg cells’ suppressive function. The screen also pointed to a strong role for another regulatory protein called ring finger protein 20 (Rnf20), which had an opposing effect. To exert these effects, Rnf20 and Usp22 seem to attach to DNA-associated protein complexes at neighboring sites within the cell’s nucleus.
Cortez met and began collaborating with Elena Montauti, a graduate student at Northwestern University, and the other lead author of the study, who was experimenting with “knock-out” mice that lack Usp22, in the Northwestern lab of pathologist and senior co-author Deyu Fang, PhD.
They found that a lack of Usp22 in Treg cells led to spontaneous development of autoimmune disease, a result of weakened Treg cells, but this deficit also hindered growth of lymphoma tumor cells. Eliminating Rnf20 in Tregs weakened by the lack of Usp22 “rescued” them, reversing at least some of the effects of Usp22 deficiency.
Study co-author Jeff Bluestone, PhD, said, “Understanding how to stabilize Treg function is a key issue in the use of cell therapy for the treatment of autoimmune diseases, organ transplantation and degenerative diseases. The research presented in this paper highlights the power of multidisciplinary collaborations and the important technological advances in CRISPR screening and T cell engineering being made by the Marson lab at UCSF to rapidly advance this potentially transformational field.”
Bluestone, emeritus professor at UCSF and former CEO of the Parker Institute for Cancer Immunotherapy, is now president and CEO of Sonoma Biotherapeutics, a San Francisco- and Seattle-based start-up that aims to develop cell therapies to treat autoimmune diseases.
“Our study highlights the power of efficient CRISPR-based screening to identify new ways to fine-tune Treg function to treat cancer or autoimmune diseases,” Cortez said. “Both Usp22 and Rnf20 are potential targets for Treg immunotherapies.”