This article is archived and only made available for historical reference. If you’d like to discover UCSF’s most recent advances in research, education and patient care, please visit the UCSF News Center.
Archive: Valley Fever Is On the Rise – But No One Knows How It Picks Its Victims
Researchers and Clinicians Are Trying to Unlock the Mystery of Why the Fungus Makes Some People So Sick and Not Others
The disease that doctors at first thought was lung cancer was likely carried on a speck of dust.
A few years ago, Kevin Pierce, a laconic retired sheriff who has lived his whole life in the Central Valley of California, went to see his family physician about some chest pains. An X-ray showed several nodules in his lungs, suggestive of a spreading cancer – not entirely surprising since Pierce is a smoker. He was referred to UCSF Fresno for treatment.
But when the doctors there investigated further, they realized the nodules in his lungs were not from cancer but from a fungal infection.
Pierce had Valley Fever, an illness caused by the fungus Coccidioides immitis, which grows in the hot, dry soil of the Central Valley and across the American Southwest.
“It’s hard to be a doctor in Fresno and not have to deal with Valley Fever,” said Michael Peterson, MD, a pulmonologist and associate dean at UCSF Fresno. In fact, Peterson said in his clinic’s experience, up to one-third of patients who are sent for biopsy to confirm lung cancer turn out instead to have Valley Fever.
In 2017, Valley Fever sent some 14,000 Americans to the doctor’s office, mostly in California and Arizona. The majority show up with flu-like symptoms and fatigue, but a small number of people develop debilitating infections that spread from the lungs to other parts of the body, including the brain. Partly because the symptoms can vary from benign to life-threatening, Valley Fever is often unrecognized even in areas where the fungus is endemic.
Before his diagnosis, Pierce had heard of Valley Fever but knew little about the disease and its treatment. “It was confusing. I really didn’t know what to think or what to expect,” he said.
Doctors are seeing more cases across California’s Central Valley and beyond, and this is leading the medical profession to confront the disease from two angles. Doctors are working to better diagnose people who may be infected. Meanwhile, scientists are working to better understand the fungus, especially basic questions like why it makes some people so sick and not others.
Shape-Shifting Fungus
This is what we know about the fungus that causes Valley Fever.
In the soil, Coccidioides immitis grows in fine filaments, which degenerate to produce spores. They are so light that any disturbance to the soil – farming, construction, even a gust of wind – can launch fragments of the fungus into the air.
Once airborne, the fungus is carried on tiny particles of dust, which can be inhaled. If it enters our lungs, it undergoes a dramatic metamorphosis.
Inside of a human body, each spore swells and develops into a spherule, a round capsule pregnant with fungal cells called endospores. These spherules can rupture, releasing endospores that turn into more spherules – and onward as the cycle of rupturing and spreading continues.
Most people struck with Valley Fever recover on their own. Some patients, like Pierce, develop lung nodules, which are small patches of infection in the lungs that can be mistaken for lung cancer. For Pierce, antifungal medications taken for a year helped him recover from the infection.
But in about 1 percent of people, the disease becomes more serious, spreading outside the lungs to infect skin, bones, and other organ systems. In the most deadly form of the disease, the fungus reaches the brain, called a meningeal infection, and patients require antifungal treatment for life.
It remains a mystery why the effects of Valley Fever vary so widely even among healthy people. Some patterns appear to be racial – African-Americans are 10 times more likely and Filipinos 175 times more likely than Caucasians to get severely sick – but the reasons, likely genetic, are still being sought by scientists.
Searching for Gaps in Our Knowledge
Anita Sil, MD, PhD, a microbiologist at UC San Francisco is working to crack this central mystery of Coccidioides: why the fungus makes some people so sick and not others.
To do so, she said, we must first learn a lot more about the basic biology of the fungus and how it behaves inside a host. “We actually know much less about fungal pathogens than we do about other types of microbial pathogens,” she said.

UCSF postdoc Bastian Joehnk suits up before entering a Biosafety Level 3 lab to study the fungus that causes Valley Fever. Strict safety precautions are followed when handling Coccidioides immitis because anyone can be infected by the airborne fungus. Photo by Noah Berger
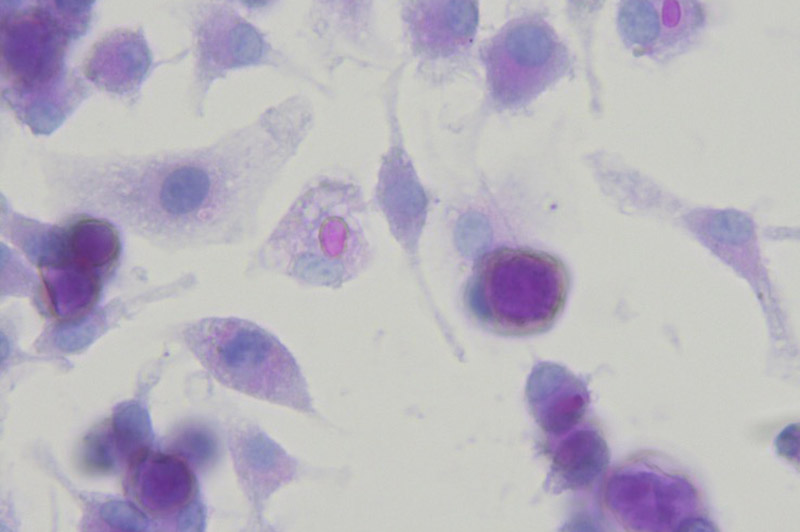
The fungus Coccidioides immitis (dark purple spheres) is shown next to macrophages (translucent cells). Image by Anita Sil laboratory
Coccidioides immitis evolved in the Americas long before humans arrived in the New World. It evolved to infect small mammals, like rodents, which may have served as precious sources of food and water in the desert. As more humans moved into these hot arid regions, farming and building in the dusty soil, the fungus infected us, too. It is one of a class of soil fungi known to cause disease and to shape-shift inside a host. In its spherule phase, the fungus is larger than the immune cells that would normally take up and destroy harmful microbes.
“When they're in the environment of the human body, these fungi really alter their growth program dramatically, and they become attuned to manipulating the human immune response and are really very good at surviving long-term in the human body,” said Sil.

Anita Sil, MD, PhD
To study how Coccidioides immitis undergoes its striking transformation, Sil’s lab is comparing samples of the fungus in its environmental form to samples of the fungus in its parasitic spherule phase.
They hope to identify the changes in gene expression that trigger the transition and also how the fungus interacts with immune cells. “Maybe having a more effective immune response, that could be one of the best weapons we could have to fight infection.”
“We want to do some fundamental research on the fungus, filling in some of our gaps in the knowledge that will ultimately impact prevention, diagnosis, and therapeutics,” said Sil.
Studying a fungus that could potentially be deadly means the researchers take no chances when handling it. Sil’s team at UCSF works with the fungus in a new, state-of-the-art Biosafety Level 3 (BSL-3) laboratory where the air is filtered completely about once a minute and every piece of equipment, even the Sharpies used to label test tubes, is sprayed down with bleach. Researchers must wear full-body protective suits with an attached air-purifying respirator, booties and two layers of gloves. No one works in the lab alone.
These precautions are necessary because the fungus infects easily through inhalation and can make even healthy people sick, said Sil.
“It's critical then to protect laboratory personnel from infection because any individual could be susceptible to infection with Coccidioides.”
An Increasing Problem
In the lab, every care is taken to prevent human contact with the fungus. But for those who live in the Central Valley and elsewhere in the Southwest, the fungus may be difficult to avoid.
Reported cases of Valley Fever have climbed in the last two decades, with a spike from 2009 to 2012, possibly due to weather conditions. The overall increase is driven by more people moving to and traveling through endemic regions and likely exacerbated by climate change that is producing drier years and more dust storms.
A recent study by UC Irvine researchers makes a grim prediction: by 2100, a warming climate will allow Valley Fever to expand throughout much of the western United States.
Even now, the fungus is almost certainly more widespread than the recorded cases. Researchers estimate that only 60 percent of infected people show symptoms. Some studies estimate that a quarter of community-acquired pneumonia in Arizona are actually Valley Fever. That means tens of thousands more people may be infected with Coccidioides immitis without knowing it.
Increasing infections will have health and financial impacts. A recent cost-of-illness study estimated that the average lifetime cost for a person diagnosed with Valley Fever approaches $94,000. For the 7,466 Californians who were diagnosed with Valley Fever in 2017, that will total nearly $700 million over their lifetimes.
7,466
Californians diagnosed with Valley Fever in 2017
$700M
Lifetime financial impacts for those diagnosed
On New Year’s day 2012, Rob Purdie of Bakersfield woke up with a pounding headache that would not go away. Two courses of antibiotics and headache medication did nothing to help and, for weeks, Purdie could do little but lie in bed in a dark room. “It consumed my life. Twenty-four hours a day for six weeks, I had one thing on my mind and it was how bad my head hurt,” he said.
Finally, a lumbar puncture confirmed that he had meningitis caused by Valley Fever. He thinks he might have picked up a spore doing yardwork in his backyard. He was put on strong doses of antifungal drugs and eventually required a port on his head to directly deliver the drugs into his brain. Some of the antifungal drugs have made his skin more sun-sensitive so he’s also had to deal with several bouts of skin cancer, and he will likely require the drugs for the rest of his life.
“What I want people to know is, if you live or travel though the Southwestern United States – Vegas or Arizona or Bakersfield or L.A. or wherever – you’re not going to travel through that part of the country without potentially coming in contact with Valley Fever,” said Purdie.
Harrowing stories like Purdie’s are raising awareness of the need for more research into Valley Fever. The disease carried on specks of dust is finally gaining attention from state officials. Last year, California approved $8 million to boost Valley Fever research and outreach, of which $3 million will go toward research across the University of California system, including the work in Sil’s lab.
“Valley Fever is very much a growing problem, and we need to be able to counteract it more effectively than we can now,” said Sil.“We have a long way to go before we’re at that point, but we hope that the knowledge we uncover will lead to new strategies to fight these infections.”
