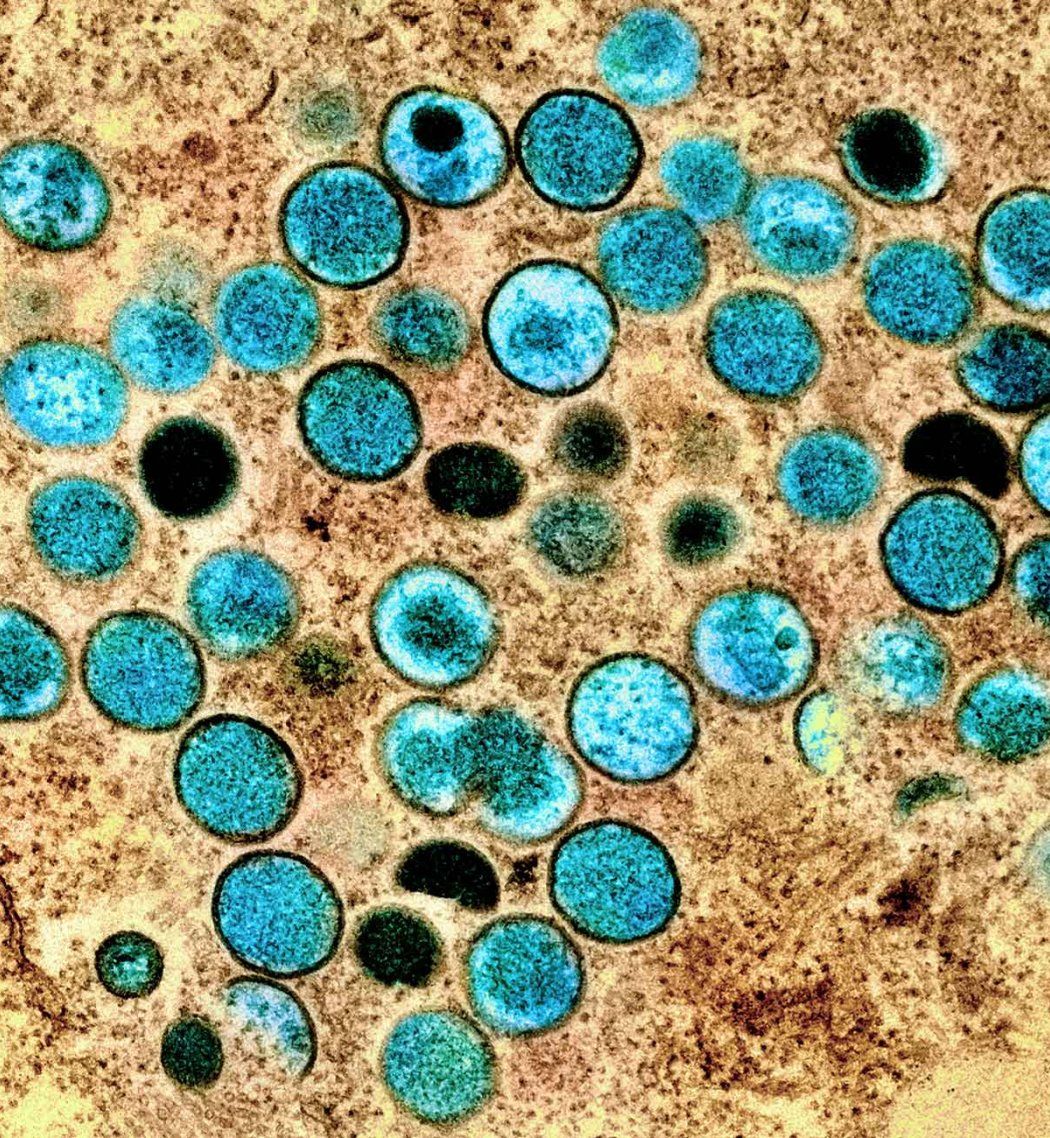
The U.S. saw more than 20,000 mpox cases and nearly six dozen deaths during the 2022 global mpox outbreak. San Francisco was hard hit. Today, mpox remains an ongoing public health emergency, according to the World Health Organization.
During the 2022 outbreak, the Centers for Disease Control and Prevention allowed physicians to prescribe it to some patients for investigational medications purposes given the lack of any approved treatments. Most physicians prescribed tecovirimat, also called TPOXX, for mpox patients — a medicine known to be effective against a close cousin of mpox, smallpox.
But did it work? Within two months of the outbreak’s start, UC San Francisco became one of the lead sites for an international clinical trial to find out. We spoke to Annie Luetkemeyer, MD, the head of UCSF’s Advancing Clinical Trials Globally (ACTG) unit, which spearheaded the research, to learn more about the virus, the trial’s result, and what it means for future pandemics.
How is mpox transmitted?
It spreads when a healthy person touches the affected skin of an infected person, and it can be sexually transmitted. In the 2022 outbreak, there was a lot of spread through sexual transmission.
There are two clades, or families, of the mpox virus. Clade 1 has traditionally been more severe and circulated largely in Central and East Africa. Clade 2 has historically been found in West Africa. A variant of Clade 2 caused the 2022 outbreak after it spread first to Europe and then the U.S.
What are the symptoms of mpox?
Mpox can be very uncomfortable and cause painful blistering and a disfiguring rash. Most often, mpox goes away on its own, and the risk of death is very low. Still, it can be quite severe and carry a risk of death, especially for children, pregnant women, and people with weak immune systems — particularly if they’re unvaccinated.
We primarily treat patients by managing pain and fever and preventing the lesions from becoming infected.
Historically, it’s been challenging to get clinical trials running during an outbreak. How did your team manage this?
We were able to start a clinical trial in under a year because of the work that had already been done to test TPOXX in a similar virus, smallpox.
What did your study find?
TPOXX was safe and well tolerated, but unfortunately, it didn’t speed up patients’ recovery time. One possible explanation for why TPOXX didn’t work is the pharmacokinetics, that is the dosing or the form in which it was given may need to be changed. It may also be that we need to give this drug in combination with another antiviral. But it’s also possible that TPOXX is simply not an effective medication for mpox, despite the promising data from animal studies on smallpox.
A study conducted largely among children in the Democratic Republic of Congo, with a different family or clade of the virus, had very similar findings.
How did including pregnant women and children in the study make it more equitable?
Pregnant women and children can be at a high risk for worse outcomes with infectious diseases, like mpox, due to weaker immune systems. Still, historically, they’re not included in many early studies for potential treatments out of an abundance of caution. Without data, drug makers can’t apply to have their medicines approved for use in these groups, so women and children sometimes have to wait years for life-saving medicines that are available to the general public.
Our trial was designed to allow inclusion of pregnant women and children in an open-label arm, along with participants who were very sick, as it was felt to be unethical to randomize people at higher risk for poor outcomes to potentially receive a placebo.
Can you explain more about how you designed the trial to do this?
Randomized controlled clinical trials are the “gold standard” in science. Randomizing is a bit like flipping a coin to pick teams: It ensures that the group or team of participants that gets a medicine is comparable to the team that doesn’t. Why? Because any characteristics that might make a person more or less susceptible to a medication, like genetics or sex, are equally represented between the two
Our study was still a randomized controlled clinical trial, but it had three arms, and only two were randomized. We didn’t randomize pregnant women, children, those with severe mpox disease or those with weak immune systems because we understood that they were at a higher risk of getting very sick. Instead, we ensured they were part of that third “open” arm of the study. This third arm enabled us to ensure that these vulnerable groups received the care they’d have received anywhere at the time, while still collecting data that will help shape future treatments for them. This was accounted for in our overall findings.
What’s next in the quest for mpox treatments?
Another smallpox drug called brincidofovir looks to be useful against mpox in laboratory tests. The Centers for Disease Control and Prevention (CDC) already allows physicians to prescribe it to patients with severe mpox, again for investigational medications purposes.
Researchers are also exploring monoclonal antibodies, or lab-engineered antibodies designed to target a specific disease, like those developed to treat COVID-19.
What does this trial tell us about the role clinical trials can play during emergencies?
Clinical trials like ours are absolutely essential during outbreaks. They allow us to evaluate whether promising investigational treatments like TPOXX are safe and effective. During mpox, we saw high demand for TPOXX for investigational medications purposes, but without data from randomized controlled studies, we couldn’t be sure of its true benefit. Our study and the research in the Democratic Republic of Congo answered this important question, demonstrating, unfortunately, that TPOXX did not improve mpox recovery time. Given this, widespread use of TPOXX is not beneficial and other strategies should be investigated.
Ultimately, trials like this give us the scientific foundation to make informed treatment decisions and continue to pursue effective treatments for current and future epidemics.