Brooklyn Haynes practically grew up at UCSF Benioff Children’s Hospital Oakland. The 27-year-old Oakland resident was diagnosed with sickle cell disease at birth and was first treated for the debilitating blood disorder when she was 2 months old.
“I like to say that Benioff Hospital Oakland raised me because I’ve been coming here since I was a baby,” Haynes said. “All of these doctors have seen me grow up. They are like my extended family — they mean the world to me.”
Haynes was a regular at the hospital’s Comprehensive Sickle Cell Center, receiving treatment sometimes several times a month from ages 2 to 23 with medications to manage pain as well as Emergency Department visits when a sickle cell crisis hit. The staff knew her so well, that they greeted her by name when she walked by.
Sickle cell disease reduces the ability of red blood cells to transport oxygen throughout the body and can cause strokes, severe organ damage and even death. It is inherited from both parents and affects approximately 100,000 Americans and millions worldwide, with a disproportionate effect on the Black community.
UCSF Benioff Hospital’s Comprehensive Sickle Cell Center has been serving patients like Haynes for 50 years. The Center celebrated its jubilee this month with a celebration at the Oakland hospital attended by the founders, employees, local and national elected officials — including U.S. Representative Barbara Lee’s office — and community advocates, such as members of the Black Panther Party. With a mission “to improve clinical outcomes and quality of life for individuals living with sickle cell disease and their families across the lifespan,” the Center not only treats communities impacted with sickle cell disease but works to increase patient access by educating providers locally, regionally and nationally — including teaching them how to partner with sickle cell specialists to avoid misdiagnoses resulting in preventable complications and deaths.
Mark Walters, MD, is principal investigator in a clinical trial to use CRISPR gene editing technology to replace the gene in the sickle cell mutation with a manufactured healthy gene using a patient’s own stem cells, which can possibly cure sickle cell disease.
Meeting a need to serve the community
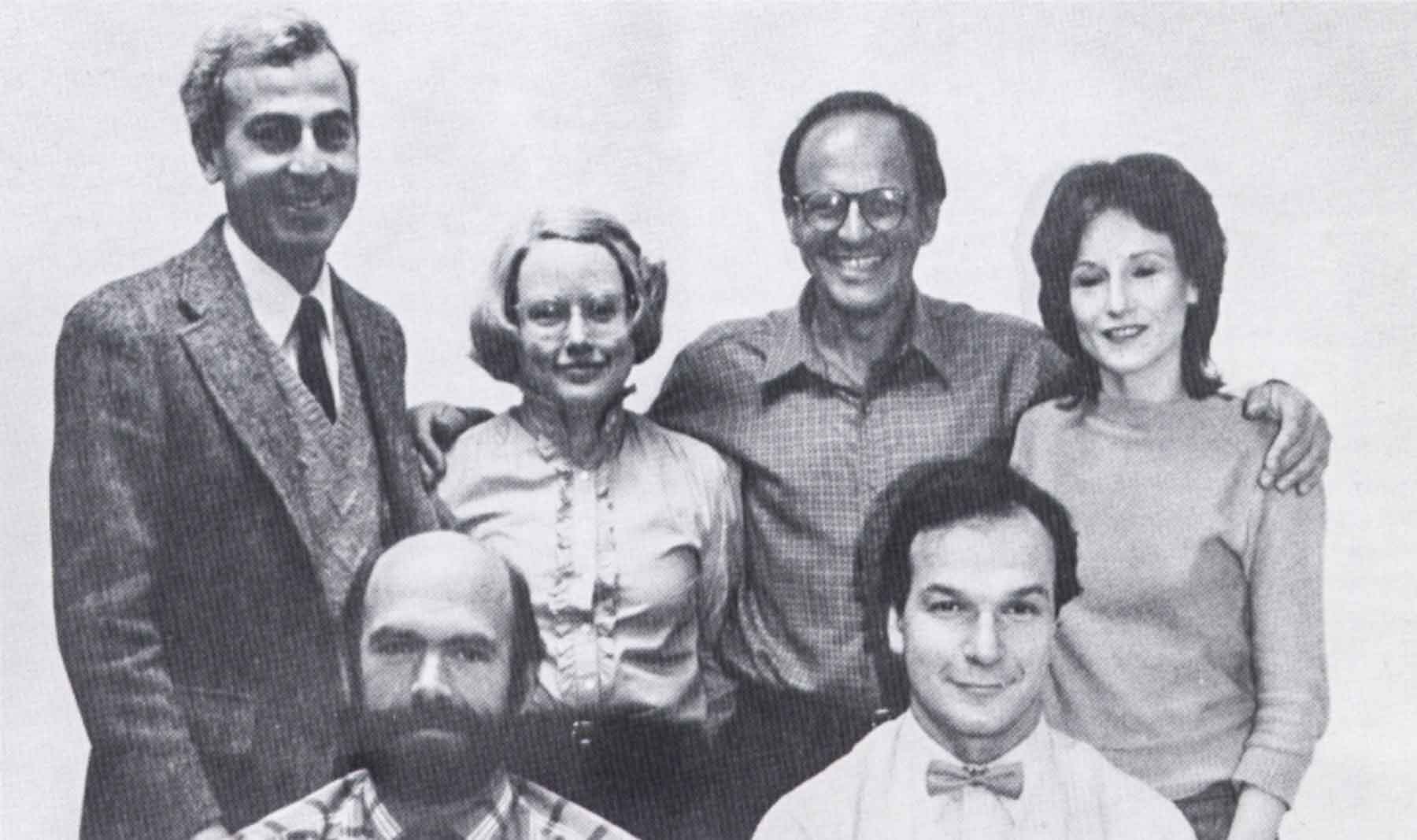
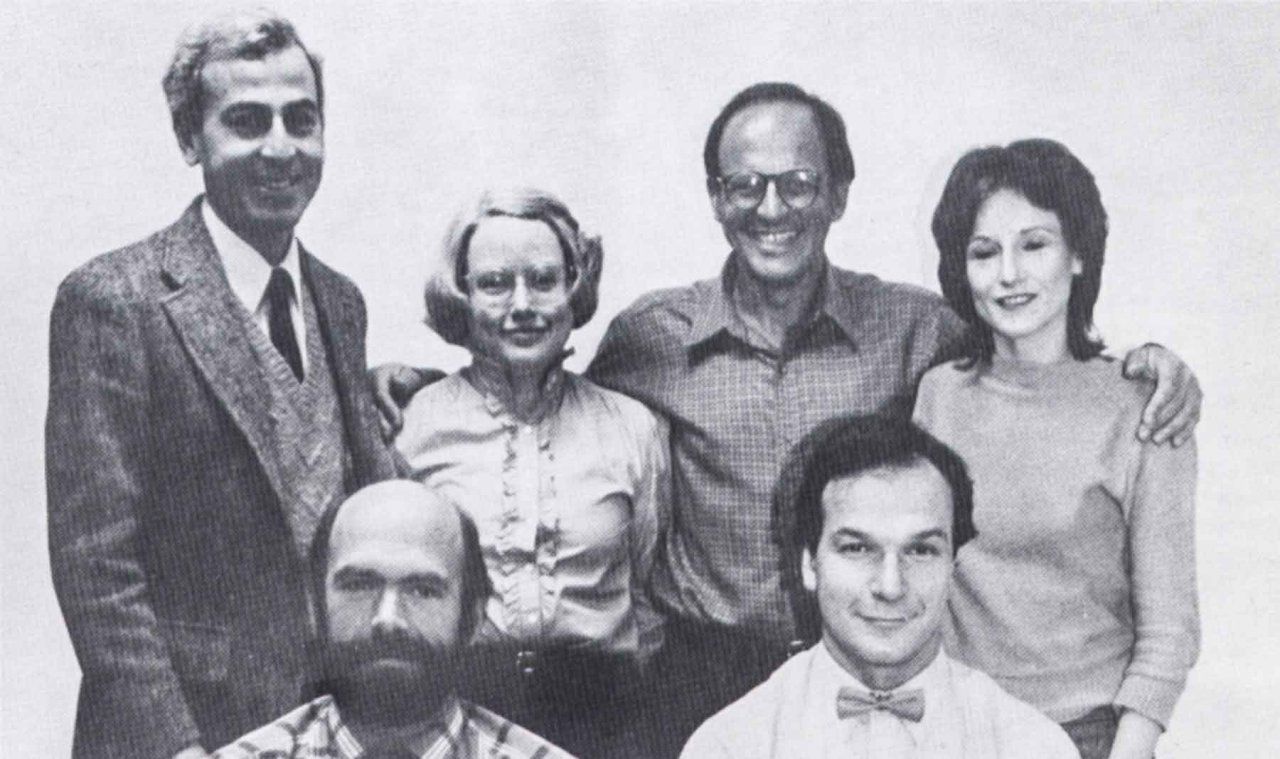
Bert Lubin, MD, late president of then Children’s Hospital Oakland, and Della Simpson, RN, saw the first patient with sickle cell disease in 1973 at Oakland’s Sickle Cell Center. At the time, support for sickle cell disease was limited, reflecting the racial biases within health care systems for a disease that primarily affected marginalized populations. Activism and advocacy by local community members, including Black clinical providers and the Black Panther Party, along with national civil rights leaders, led to the Sickle Cell Anemia Control Act — aimed at ending discriminatory testing practices and requiring volunteer screening.
Oakland’s Sickle Cell Center was one of the first federally funded programs in the country to provide comprehensive diagnosis, treatment, community education and long-term health management for children and adults with sickle cell disease. Now known as the UCSF Sickle Cell Center of Excellence, it is recognized as one of the largest and most comprehensive sickle cell programs in the Western United States and is a national leader at almost every level.
“We believed we should be there for patients with sickle cell disease for their entire lifespan.”
- Elliott Vichinsky, MD


“We believed we should be there for patients with sickle cell disease for their entire lifespan,” said Elliott Vichinsky, MD, who was recruited by Lubin from University of Washington in 1978 to lead the Center. “Adults had nowhere else to go where their condition was understood and properly treated.”
The unusual arrangement of a pediatric hospital that treats adults came about because of insulting and even dehumanizing patient experiences that many adults with sickle cell disease encountered at other hospitals — Haynes among them. When she was 23, Haynes transitioned out of the Oakland pediatric hospital to adult care at a different area hospital. Her nightmares were realized when checking into an emergency room for a sickle cell crisis — an excruciating episode involving high levels of pain requiring high doses of pain medications.
“As an adult, they automatically think that you’re a drug seeker just because you know your pain medication regimen so well,” she said. “Of course, we know what pain medications we need. We’ve been doing this our whole life and all we know is pain. At Children’s Oakland, they knew my regimen and knew exactly what to do to get me through.”
A history of sickle cell innovation
UCSF Benioff Oakland was among the first pediatric hospitals in the country to provide newborn screening for sickle cell disease and continues to lead the way with advances in research and therapies. The sickle cell team has conducted clinical trials for stroke prevention, a primary side effect of sickle cell, and led trials for FDA approval of Voxelotor, one of the most common sickle cell drugs on the market. In 2021, the team received $17 million in funding — the largest grant in the history of the Oakland hospital — to use CRISPR gene editing technology to replace the sickle-cell-causing gene with a manufactured healthy gene using a patient’s own stem cells. The technology, a collaboration with UCSF, UCLA and Nobel Laurate Jennifer Doudna, PhD’s lab — the Innovative Genomics Institute at UC Berkeley — has shown in early testing to be a possible cure for the disease.
“This therapy has the potential to transform sickle cell disease care,” said Mark Walters, MD, professor of Pediatrics at UCSF and principal investigator of the clinical trial. “If this is successfully applied in young patients, it has the potential to prevent irreversible complications of the disease.”
For Brooklyn Haynes, the new treatment sounds promising but she’s careful about her expectations at this early stage.
“When I first heard about the CRISPR trial, I’m not going to lie, I was excited because it’s sounds really good,” she said. “I don’t want to get my hopes up though. I’m just curious to see how far this can go.”
For now, Haynes appreciates the care and respect she has received as a patient at UCSF Benioff Oakland.
“These doctors and these nurses here, they really care,” she said. “And that’s not something you find every day.”
Meeting a need to serve the community
Bert Lubin, MD, late president of then Children’s Hospital Oakland, and Della Simpson, RN, saw the first patient with sickle cell disease in 1973 at Oakland’s Sickle Cell Center. At the time, support for sickle cell disease was limited, reflecting the racial biases within health care systems for a disease that primarily affected marginalized populations. Activism and advocacy by local community members, including Black clinical providers and the Black Panther Party, along with national civil rights leaders, led to the Sickle Cell Anemia Control Act — aimed at ending discriminatory testing practices and requiring volunteer screening.
Oakland’s Sickle Cell Center was one of the first federally funded programs in the country to provide comprehensive diagnosis, treatment, community education and long-term health management for children and adults with sickle cell disease. Now known as the UCSF Sickle Cell Center of Excellence, it is recognized as one of the largest and most comprehensive sickle cell programs in the Western United States and is a national leader at almost every level.
“We believed we should be there for patients with sickle cell disease for their entire lifespan.”
- Elliott Vichinsky, MD
“We believed we should be there for patients with sickle cell disease for their entire lifespan,” said Elliott Vichinsky, MD, who was recruited by Lubin from University of Washington in 1978 to lead the Center. “Adults had nowhere else to go where their condition was understood and properly treated.”
The unusual arrangement of a pediatric hospital that treats adults came about because of insulting and even dehumanizing patient experiences that many adults with sickle cell disease encountered at other hospitals — Haynes among them. When she was 23, Haynes transitioned out of the Oakland pediatric hospital to adult care at a different area hospital. Her nightmares were realized when checking into an emergency room for a sickle cell crisis — an excruciating episode involving high levels of pain requiring high doses of pain medications.
“As an adult, they automatically think that you’re a drug seeker just because you know your pain medication regimen so well,” she said. “Of course, we know what pain medications we need. We’ve been doing this our whole life and all we know is pain. At Children’s Oakland, they knew my regimen and knew exactly what to do to get me through.”
A history of sickle cell innovation
UCSF Benioff Oakland was among the first pediatric hospitals in the country to provide newborn screening for sickle cell disease and continues to lead the way with advances in research and therapies. The sickle cell team has conducted clinical trials for stroke prevention, a primary side effect of sickle cell, and led trials for FDA approval of Voxelotor, one of the most common sickle cell drugs on the market. In 2021, the team received $17 million in funding — the largest grant in the history of the Oakland hospital — to use CRISPR gene editing technology to replace the sickle-cell-causing gene with a manufactured healthy gene using a patient’s own stem cells. The technology, a collaboration with UCSF, UCLA and Nobel Laurate Jennifer Doudna, PhD’s lab — the Innovative Genomics Institute at UC Berkeley — has shown in early testing to be a possible cure for the disease.
“This therapy has the potential to transform sickle cell disease care,” said Mark Walters, MD, professor of Pediatrics at UCSF and principal investigator of the clinical trial. “If this is successfully applied in young patients, it has the potential to prevent irreversible complications of the disease.”
For Brooklyn Haynes, the new treatment sounds promising but she’s careful about her expectations at this early stage.
“When I first heard about the CRISPR trial, I’m not going to lie, I was excited because it’s sounds really good,” she said. “I don’t want to get my hopes up though. I’m just curious to see how far this can go.”
For now, Haynes appreciates the care and respect she has received as a patient at UCSF Benioff Oakland.
Milestones through the decades
1973
Della Simpson, RN and Bert Lubin, MD see the first patient with sickle cell disease at Oakland's Sickle Cell Center
1974
First NIH supported Sickle Cell Screening, Counseling and Education Program
1975
NHLBI Comprehensive Sickle Cell Center established
Elliott Vichinsky, MD and Bert Lubin, MD, initiate California’s Newborn Hemoglobin Screening Program
1984
First blood and bone marrow transplant cures a case of sickle cell disease
1986
The prophylactic penicillin study tests whether daily administration of oral penicillin would reduce bacterial infections in children with sickle cell
1995
Multicenter Study of Hydroxyurea investigates the use of hydroxyurea as a sickle cell treatment. Hydroxyurea increases the production of fetal hemoglobin, and was found to reduce the severity and frequency of pain crises, decrease the need for blood transfusions, and improve the overall health of sickle cell patients. The trial established hydroxyurea as a standard treatment for sickle cell disease
1997
The Stroke Prevention Trial investigates the effectiveness of blood transfusion therapy in preventing strokes in children with sickle cell disease, as well as the benefits and risks of long-term blood transfusion therapy such as iron overload
2010
A study demonstrates adults with sickle cell may have changes in brain function
2019
Voxelotor is introduced as the third FDA approved disease modifying therapy for sickle cell disease
2021
The largest grant in Benioff Hospital Oakland history is awarded to Mark Walters, MD, for a gene editing trial