A new UC San Francisco-led study brings scientists closer to understanding the causes of a mysterious rash of cases of acute severe hepatitis that began appearing in otherwise healthy children after COVID-19 lockdowns eased in the United States and 34 other countries in the spring of 2022.
Pediatric hepatitis is rare, and doctors were alarmed when they started seeing outbreaks of severe unexplained hepatitis. There have been about 1,000 cases to date; 50 of these children needed liver transplants and at least 22 have died.
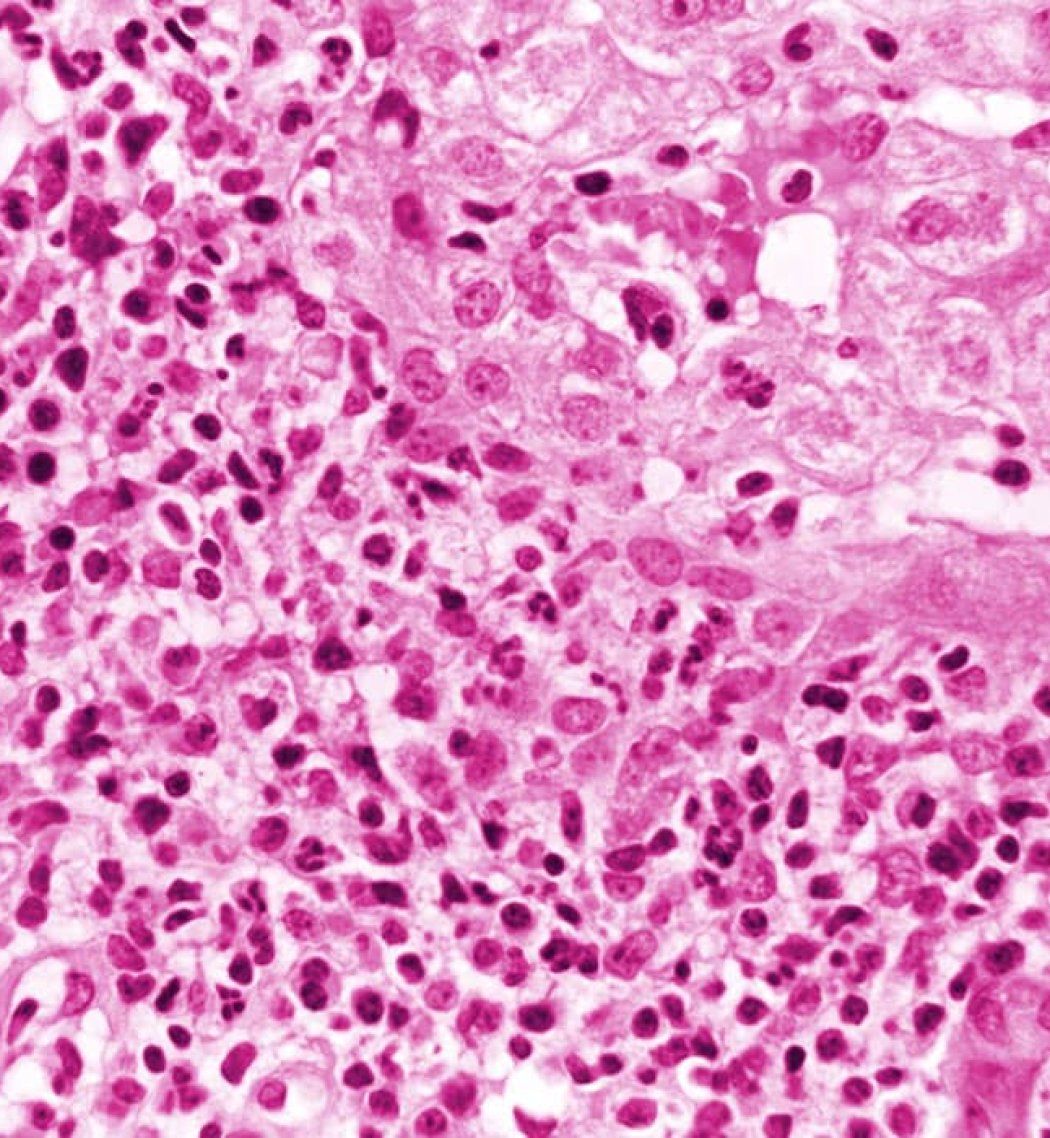
In the study, publishing on March 30 in Nature, researchers linked the disease to co-infections from multiple common viruses, in particular a strain of adeno-associated virus type 2 (AAV2). AAVs are not known to cause hepatitis on their own. They need “helper” viruses, such as adenoviruses that cause colds and flus, to replicate in the liver.
Once they returned to school, children were more susceptible to infections with these common pathogens. The study suggests that for a small subset of these children, getting more than one infection at the same time may have made them more vulnerable to severe hepatitis.
“We were surprised by the fact that the infections we detected in these children were caused not by an unusual, emerging virus, but by common childhood viral pathogens,” said Charles Chiu, MD, PhD, professor of laboratory medicine and medicine in the Division of Infectious Diseases, director of the UCSF Clinical Microbiology Laboratory, and senior author of the paper.
“That’s what led us to speculate that the timing of the outbreak was probably related to the really unusual situations we were going through with COVID-19 related school and daycare closures and social restrictions,” Chiu said. “It may have been an unintended consequence of what we have experienced during the last two-to-three years of the pandemic.”
By August 2022, clusters of cases were reported in 35 countries, including the U. S., where 358 cases were under investigation. The Centers for Disease Control and Prevention (CDC) launched an investigation into the causes.
Testing for Viruses
To conduct the study, which was backed by the CDC, researchers used polymerase chain reaction (PCR) along with various metagenomic sequencing and molecular-testing methods to examine plasma, whole blood, nasal swab and stool samples from 16 pediatric cases in six states – Alabama, California, Florida, Illinois, North Carolina and South Dakota – from Oct. 1, 2021, to May 22, 2022. The specimens were compared with 113 control samples.
... The infections we detected in these children were caused not by an unusual, emerging virus, but by common childhood viral pathogens.
In genotyping the 14 available blood samples, adeno-associated virus 2 (AAV2) was detected in 93% of the cases and human adenoviruses (HAdVs) were found in all the cases; a specific type of adenovirus linked to gastroenteritis (HAdV-41) was found in 11 cases. Additional co-infections with Epstein-Barr, herpes and enterovirus were found in 85.7% of cases.
Chiu noted the results mirrored the findings of two concurrent studies conducted in the United Kingdom, which identified the same AAV2 strain. All three studies identified co-infections from multiple viruses, and 75% of the children in the U.S. study had three or four viral infections.
Since AAVs are not considered pathogenic on their own, a direct causal link with the severe acute hepatitis has yet to be established. The study notes, however, that children may be especially vulnerable to more severe hepatitis triggered by co-infections. While infections from adeno-associated viruses can occur at any age, the peak is typically between 1 and 5 years old, and the median age of the affected children in the study was 3 years old.
The clusters of acute severe hepatitis in children have recently waned, but Chiu said the best way to protect children from this unlikely outcome is by washing hands frequently and staying home when sick.
Authors: In addition to Chiu, authors include Venice Servellita, BS/CLS, Alicia Sotomayor Gonzalez, PhD, of UCSF, and Daryl Lamson of the New York State Department of Public Health. Please see the study for additional authors.
Funding: The study was funded in part by the U.S. Centers for Disease Control and Prevention (contracts 75D30121C12641 and 75D30121C10991 C.Y.C.) and the Biomedical Advanced Research and Development Authority (BARDA) (contract 75A50122C00022), and the National Institutes of Health/National Institute of Child Health and Human Development (grant R61HD105618 C.Y.C. and C.A.R.). Additional funding was awarded under Agreement No. HSHQDC-15-C-00064 to Battelle National Biodefense Institute by the Department of Homeland Security, Science and Technology Directorate, for the management and operation of the National Biodefense Analysis and Countermeasures Center.
Disclosures: Please see the paper for a complete list of disclosures.