A sexual health strategy called doxy-PEP, in which people who have a history of sexually transmitted infections (STIs) take doxycycline after condomless sex, is highly effective. But it is still associated with a limited rise in resistant strains of bacteria, according to preliminary results presented at 2023 CROI of a study led by UC San Francisco, the San Francisco Department of Public Health and the University of Washington.
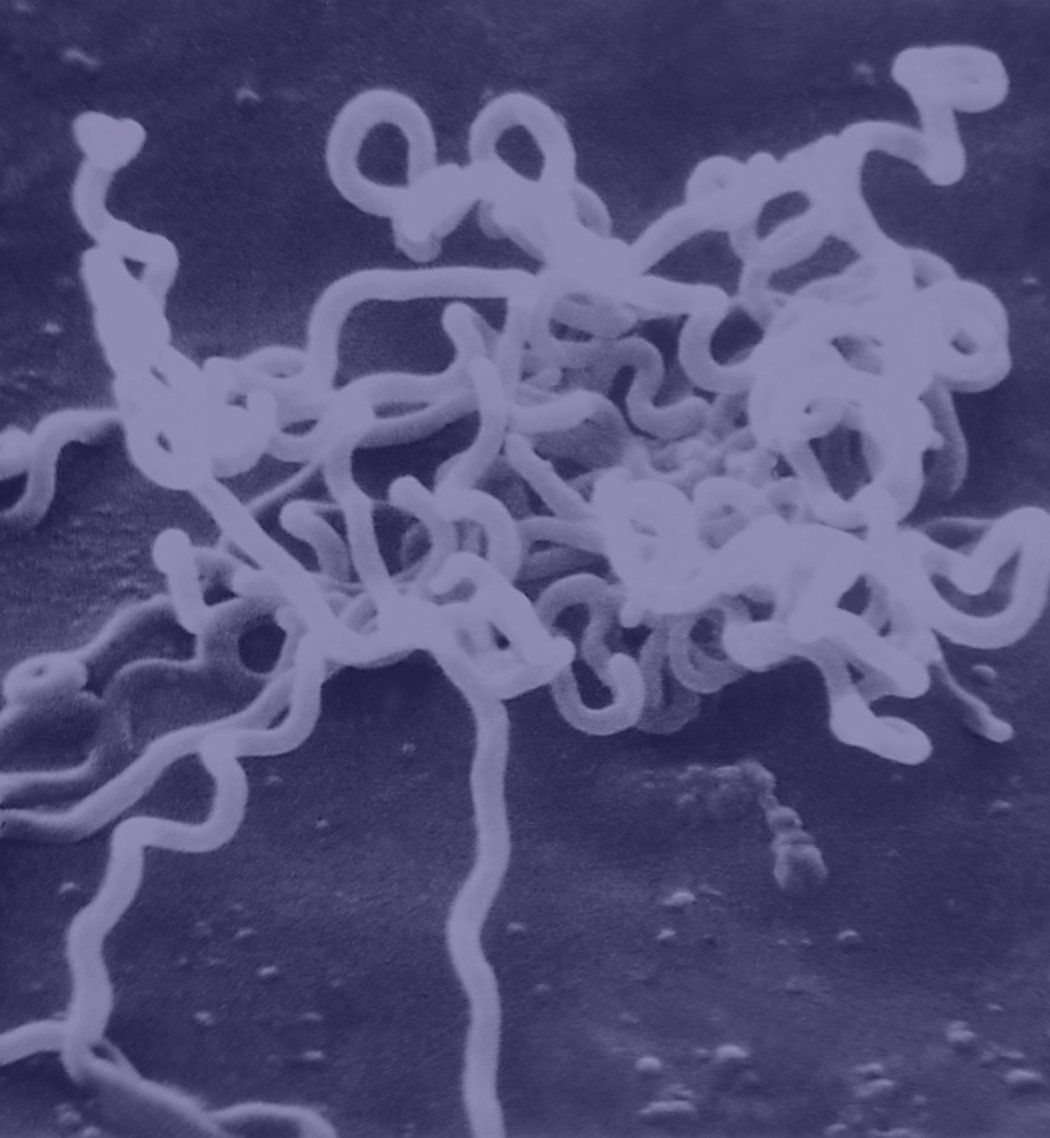
Doxy-PEP stands for doxycycline post-exposure prophylaxis. It involves taking one 200mg pill of doxycycline, a kind of tetracycline, as soon as possible but no later than three days after having sex without a condom. The study observed its effects over the course of a year in men who have sex with men (MSM) and transgender women and found it reduced bacterial STIs, specifically gonorrhea, chlamydia and syphilis, by two-thirds each quarter.
The researchers said they were encouraged to find the effects on antibiotic resistance appear to be small thus far, although more time is needed to know the extent and trajectory of antimicrobial resistance associated with intermittent doxycycline use.
New strategies are urgently needed to curb STIs, which have been on the rise for several decades among men who have sex with men. STIs are also increasing among women, for whom rising syphilis rates are of particular concern. The complications for babies born to mothers infected with syphilis can be severe, including death and loss of vision and hearing. In rare cases, adults with syphilis can become blind and deaf if not diagnosed and treated.
Researchers stressed the approach is meant for men and transgender women with a risk for recurrent STIs, treatment of which requires exposure to antibiotics. To qualify for the study, participants had to have at least one occurrence of gonorrhea, chlamydia or syphilis in the past year, along with a history of condomless sex with a male partner.
“This isn’t a choice between antibiotics and no antibiotics in men and transgender women with a history of recurrent STIs,” said Annie Luetkemeyer, MD, professor of infectious diseases at Zuckerberg San Francisco General Hospital and UCSF, a co-principal investigator on the study. “The alternative here for many is repeated STIs that lead to recurrent antibiotics. Doxy-PEP may mitigate the amount of antibiotics used, including broader spectrum antibiotics like ceftriaxone, the use of which was reduced by 50% in those taking doxy-PEP.”
The presentation at 2023 CROI, given on Feb. 20, examined antimicrobial resistance during doxy-PEP use in gonorrhea and two other types of bacteria, Staphylococcus aureus that lives on the skin and non-disease-causing Neisseria species that live in the throat.
When the researchers looked at a subset of the participants who were diagnosed with gonorrhea while they were in the study, they found more tetracycline resistant gonorrhea in those on doxy-PEP than in those who were not taking it (30% vs 11%). This suggests that doxy-PEP may be less protective against strains of gonorrhea that already have tetracycline resistance. Larger population-based studies will be needed to understand if doxy-PEP use increases tetracycline resistance in gonorrhea.
Taking doxy-PEP affected the extent to which participants were “colonized” by Staphylococcus aureus, which can be associated with subsequent clinical Staph infections. Doxy-PEP reduced colonization from 44% to 31%, but the cultures that were resistant to doxycycline went up from 5% to 13%, a small but statistically significant increase. There was no increase in the presence of methicillin resistant Staphylococcus aureus (MRSA) overall or with doxycycline-resistant MRSA. This is important because doxycycline is sometimes used to treat MRSA.
Neisseria species commonly live in the throat without causing disease and can be a reservoir for resistance genes that can then be passed to disease causing bacteria. Neisseria species did not appear to be affected by doxy-PEP use; doxycycline resistance was already present in about two-thirds of these bacteria, and this did not change significantly after 12 months of doxy-PEP.
The ZSFG HIV clinic and the SF City Clinic, operated by SFDPH, will continue evaluating the effect of doxy-PEP on the gut microbiome, as well as the other STIs, such as mycoplasma genitalium and chlamydia.
“Doxy-PEP is a promising strategy to reduce sexually transmitted infections in populations that are disproportionately affected by high rates of sexually transmitted infections, specifically, men who have sex with men and transgender women who have had recent STIs,” said Connie Celum, MD, professor of global health, medicine, and epidemiology at the University of Washington, a co-principal investigator on the study. “It will be important to monitor the impact of doxy-PEP on antibiotic resistance over time and weigh this against the demonstrated benefit of reduced STIs.”
Funding: The trial was funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, through grant R01AI143439, and conducted at the HIV clinic at Zuckerberg San Francisco General Hospital and the San Francisco City Clinic, both part of the San Francisco Department of Public Health, and the Madison Clinic and the Sexual Health Clinic at Harborview Medical Center, both at the University of Washington
The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. It includes UCSF Health, which comprises three top-ranked hospitals, as well as affiliations throughout the Bay Area. Visit ucsf.edu, or see our Fact Sheet.