Cardiology Conference Features UCSF Health Experts
Prestigious Medical and Scientific Meeting Highlights Cutting Edge Research and Treatment of Cardiovascular Disease
Cardiology experts from UCSF Health will present new research and clinical findings at the American College of Cardiology’s (ACC) Annual Scientific Session & Expo in Washington, DC, April 2 to 4, 2022. The 71st annual conference brings together leading cardiology researchers and clinicians, helping to shape clinical practices and research directions for a global audience. The conference will also have a virtual component in addition to the in-person gathering.
This year’s scientific program features the latest developments in clinical research by experts from the UC San Francisco’s Division of Cardiology. UCSF investigators and clinicians will participate in oral, moderated poster and traditional poster presentations in such areas as Cardio-Oncology, Interventional and Structural Cardiology, Endovascular Therapies, Global Cardiovascular Health, Electrophysiology, Acute Coronary Syndrome, AI in Cardiovascular Imaging, and Peri-operative Care Strategies.
Here are some highlights:
2022 Young Author Achievement Award: Connor G. O’Brien, MD, UCSF assistant professor of Medicine and cardiologist with expertise in echocardiography and critical care medicine, will receive ACC’s Young Author Achievement Award. The award is presented to researchers within the first five years of their training in the areas of clinical investigations, basic and translational science and outcomes research. O’Brien’s 2021 study focused on the role of mesenchymal stem cells (MSCs) in treating anthracycline-induced cardiomyopathy (AIC) in cancer survivors. The study evaluated data during the SENECA trial, finding a mechanism by which MSCs could improve cardiovascular performance in AIC independent of regeneration, and inform future trial design evaluating the therapeutic potential of MSCs. O’Brien will receive the award at conference during the JACC Editorial Board Meet and Greet on Sunday, April 3.
The Harms Associated with Inferior Vena Cava Filters: Rachel Warren, BA, Sanket S. Dhruva, MD, Madris Kinard, MBA, John Neuhaus, PhD, Rita F. Redberg, MD, MS analyzed data related to concerns about Inferior Vena Cava filters (IVCF) that have been utilized since the 1970s for patients with venous thromboembolism who have contraindications to anti-coagulation. Despite limited supporting efficacy data and increasing safety concerns following an FDA safety advisory in 2010, rates of IVCF implantation in the U.S. remain high, and most retrievable IVCF are never removed. This study sought to characterize and update data about the safety of IVCF. The study found an apparent increase in rate of adverse events for IVCF, despite the well-established under-reporting to MAUDE – the FDA’s adverse event reporting database – highlighting the ongoing risks associated with continued use of these devices. View session abstract: 1013-07
Atrial Fibrillation and Race in The United Kingdom: Katrine Emilie Frimodt-Møller, MS, Gregory Nah, MA, Tor Biering-Sorensen, MD, PhD, MPH, Francesca Delling, MD, MPH, Gregory M. Marcus, MD, MAS. Within the US, whites experience a higher risk of atrial fibrillation (AF) compared to other races despite harboring less conventional risk factors, and while the reasons remain unknown, they could be related to differential access to healthcare. The United Kingdom (UK) provides socialized medicine, providing equal access to healthcare regardless of race. Leveraging longitudinal data from the UK biobank that categorized patients as white, black, South Asian, Chinese, or multiracial, the researchers found whites experienced a heightened risk of AF compared to other races in a large community-based population outside the US, suggesting this may be a global phenomenon most pertinent to race rather than differences in healthcare access or other environmental influences. View session abstract: 1342-128/128
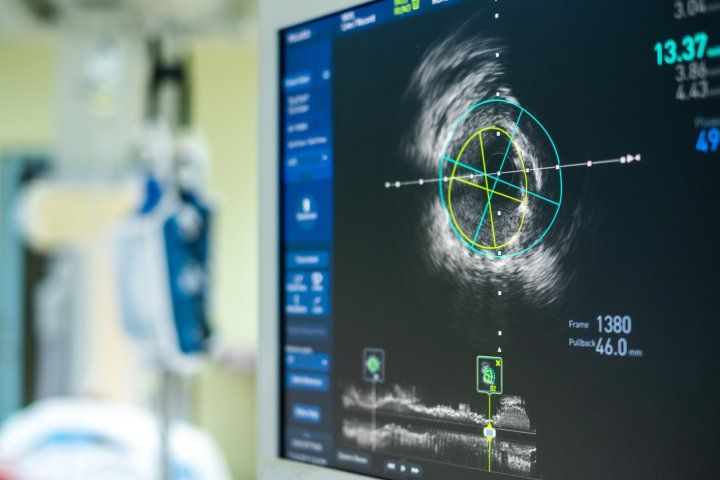
Intracardiac Echocardiography As An Adjunct For Off-Label Edge-To-Edge Repair Of The Tricuspid Valve: Gregory Judson, MD, David Blusztein, MD, Punita Kaveti, MD, Tom C. Nguyen MD, FACS, FACC, Tobias Deuse, MD, Hope Caughron, MD, Atif Qasim, MD, MS, Kirsten Tolstrup, MD, Vaikom S. Mahadevan, MD, FACC evaluated the safety and effectiveness of Transcatheter edge-to-edge (TEER) tricuspid valve (TV) repair with the Mitraclip system (TV TEER) for patients with severe tricuspid regurgitation (TR) at high risk for surgery. Patients with severe TR who underwent successful TV TEER were evaluated and intracardiac echocardiography (ICE) was used at the discretion of the primary operator. The study demonstrates real-world procedural effectiveness of TEER for severe TR with adjunct ICE for patients at high surgical risk. View session abstract: 1168-002/2
Standard Versus Intensive Monitoring Post-Myocardial Infarction Looking for New-Onset Atrial Fibrillation or Flutter: Christopher Cheung, MD, MPH (UCSF Cardiac Electrophysiology Fellow) and researchers from University of British Columbia sought to evaluate whether a long-term electrocardiogram (ECG) monitoring strategy is superior to conventional follow-up for atrial fibrillation (AF) detection in patients following acute coronary syndrome (ACS). The multi-center, randomized clinical trial included patients with no evidence of AF, who presented to hospital with a myocardial infarction (MI). The primary outcome was newly detected AF or atrial flutter (AFL) within 30 days of enrollment in the study. The researchers found that intensive monitoring was superior to conventional follow-up for detecting new-onset AF/AFL following presentation with ACS. This abstract is a finalist for the American College of Cardiology Young Investigator Award. View session abstract: 908-7
The Effect of Low Perfusion Pressure on The Frequency and Complexity of Ventricular Fibrillation in Isolated Contracting Hearts: Namita Ravi, BS, Jan Lebert, MS, Jan Christoph, PhD used optical mapping (OM) help uncover the electrical patterns of ventricular fibrillation (VF). The researchers used a novel motion-tracking algorithm to study VF response to perfusion pressure in ex vivo contracting hearts. The study found lower perfusion pressure results in more organized VF in contracting hearts. View session abstract: 1028-03
Francesca Delling, MD, MPH, will present TEE for DCCV: Thrombus versus SEC vs Artifact (632-04) during Session 632: “Imaging in EP Procedures: Smoke and Mirrors?” Additionally, Kirsten E. Fleischmann MD, MPH will chair Session 804: “Core Knowledge in Action: What Are the Current Recommendations for Risk Stratification of Non-cardiac Surgery Patients?” and present “What Would Updated Guidelines Say About Perioperative Diagnostic Testing?” during Session 703: Peri-operative Care for Non-Cardiac Surgery: Emerging Strategies and Ongoing Controversies.” Rima Arnaout, MD will present Deep Learning Models of the Echocardiogram (690-04) during Session 690: “Artificial Intelligence and Machine Learning in Cardiovascular Imaging.”
For a complete list of ACC22 abstracts, please see: https://www.abstractsonline.com/pp8/#!/10461