AIDS at 40: How HIV and COVID-19 Are Informing Our Responses to Both Pandemics
This story is one in a series of first-person perspectives from those who are working on the frontlines to better understand, treat and prevent transmission of HIV and AIDS as well as COVID-19. You can read more about the 40 years of AIDS in SF and how it has shaped the COVID-19 response.

Monica Gandhi, MD
Reflecting on the 40th anniversary of the first description of AIDS in the MMWR on June 5, 1981, is profoundly moving for me as a member of UC San Francisco’s HIV community for so many years. AIDS informed COVID-19 and COVID-19 will inform AIDS and our response to pandemics will be ever shaped by UCSF.
Why was it my dream for so long to come to UCSF? I grew up Indian-American in the public school system in Salt Lake City – elementary, middle school, high school – in the 1970s and ’80s. There was not much diversity in Salt Lake City at the time, and there was a feeling of isolation and of stigma from something I could not help, which was the color of my skin.
These feelings from early on led to my long-standing passion for working in a disease, specifically HIV, which tends to single out the “other,” the stigmatized, the poor and the disenfranchised. Going to India when I was growing up also put into sharp focus for me that disparities in health outcomes, particularly from basic infectious diseases that could and should have receded a long time ago, are fueled by disparities between the rich and poor.
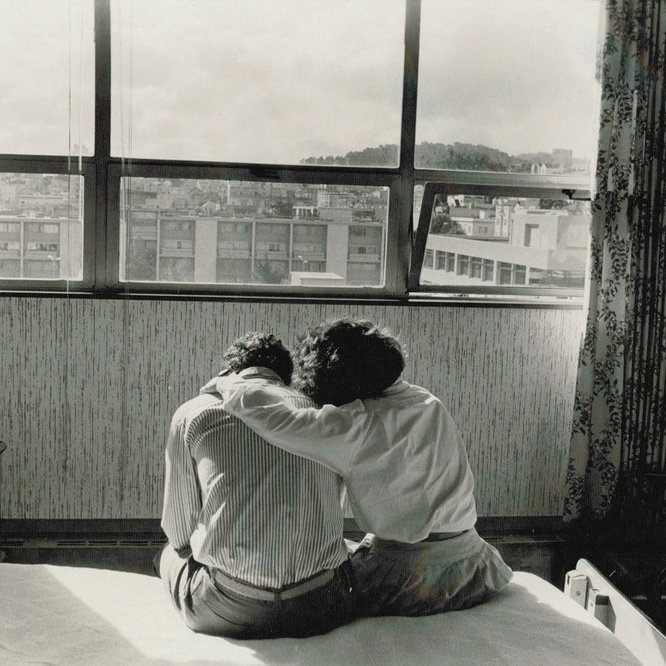
I then went to Harvard Medical School but made a beeline for UCSF for medical residency and Infectious Diseases fellowship, as I knew this was the place where the first AIDS outpatient clinic (Ward 86) had been established at San Francisco General Hospital. It’s where nurses and doctors across the campuses did not stigmatize, but held AIDS patients’ hands while they were dying; where I would learn to be an HIV doctor, somehow – for so many years – the only thing I wanted to be.
AIDS informed COVID-19 and COVID-19 will inform AIDS and our response to pandemics will be ever shaped by UCSF.
And, indeed, I learned how to be an HIV doctor here at UCSF, from Harry Hollander, Paul Volberding, Eric Goosby, Steve Deeks, Diane Havlir, Meg Newman, Jay Levy, Mark Jacobson, Laurence Huang, Diane Jones, Mary Lawrence Hicks, and so many others. I learned about compassion, courage, dedication to a cause and advocacy. I grew up here at UCSF and eventually had the honor of becoming the medical director of the Ward 86 HIV Clinic in 2014 and the director of our Center for AIDS Research in 2019. And along the way, I learned that to be an HIV doctor was to be an activist, a realization that was to be tested for all of us in 2020.
When COVID-19 washed across the world in 2020 and hit our city in March of that year, I remember looking around at all of the people who trained me at UCSF and wondering how we would all respond. Eric Goosby, MD, went to work on the Biden campaign and eventually joined the Biden-Harris Transition COVID-19 Advisory Board. Diane Havlir, MD, immediately re-created her amazing SEARCH campaign (from East Africa) in the Mission District in San Francisco and started testing, and then, eventually vaccinating the community. Paul Volberding, MD, educated us through his work with the International AIDS Society-USA and Steven Deeks, MD, turned to the immune system, once again, for COVID-19 as he had with HIV. Jay Levy, MD, and I had talks of T cell immunity to the vaccines and to natural infection and how to calm the public discourse around COVID-19 variants.
And many of us became activists once again: on why the disproportionate impact of COVID-19 on poor communities was recapitulating what happened in HIV; on how harm reduction (a principle where you try to mitigate new infections by understanding human needs in your recommendations) over abstinence worked for HIV and should be applied to COVID-19 mitigation; on how school closures were leading to mental health effects in the children of our city and nation; and how “vaccine hesitancy” was to be met with compassionate community-based education and a willingness to listen.
We are now watching the COVID-19 epidemic recede in rich countries, including our own, and rise in poor countries, despite having the solution of vaccines in hand. This disparity is achingly similar to how it felt to be an HIV doctor in the late ’90s and early 2000s, when life-saving antiretroviral therapy (ART) was only available to wealthy nations, and not poor. The need for global vaccine equity is our next battle, and UCSF – as always – is rallying to the cry. It has been my honor to be at UCSF since 1996 and to learn from the great leaders in our HIV community.
I met my late husband (Rakesh Mishra) during my medical residency at UCSF; he trained in Cardiology here and came back to serve on faculty at the San Francisco VA, only to die of cancer in late 2019. My two children were born at UCSF. I have known loss and incredible grief at UCSF, but I have also known resilience. I have seen it in my patients and in the HIV researchers, clinicians and educators here at UCSF, and it has been one of the greatest privileges of my life to serve along with them as we defeat COVID-19 and turn back to eradicating HIV/AIDS in our lifetime.
Monica Gandhi, MD, MPH, is an infectious disease specialist who serves as Chief of the Division of HIV, Infectious Diseases, and Global Medicine at UCSF/ Zuckerberg San Francisco General Hospital. She also serves as the Director of the UCSF Center for AIDS Research and the Medical Director of the HIV Clinic at SFGH known as “Ward 86.”
40 Years of AIDS in SF
Learn about UCSF’s four decades of work in HIV and AIDS, and how it has informed our response to the COVID-19 pandemic.