Triple-Negative Breast Cancers Depend on Fat as Fuel, Research Shows
UCSF Scientists Halt Growth of Challenging Tumors With Drug That Blocks Fatty Acid Metabolism
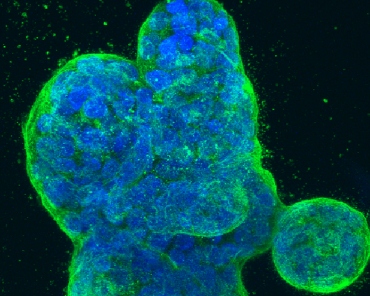
The most intractable common form of breast cancer might in most cases be treatable by drugs that target fat metabolism, according to UC San Francisco researchers who discovered the tumors’ frequent dependence on fat as an energy source, and then successfully treated human breast tumors that they transplanted and grew in mice.
Roughly one-in-five invasive breast cancers are categorized as triple negative, meaning they do not rely on the hormones estrogen and progesterone for growth, nor on human epidermal growth factor receptor 2 (HER2). Given this, they are not vulnerable to modern hormonal therapies or to the HER2-targeted drug Herceptin (trastuzumab). Because they grow rapidly in early stages, triple-negative breast tumors often respond well initially to older chemotherapies that kill dividing cells, but a greater percentage of women diagnosed with this type of breast cancer die within five years of diagnosis because of the emergence of cancer metastasis.
Apparent Source of Energy
In a new study published online on March 7 in Nature Medicine, researchers led by breast oncologist Andrei Goga, MD, PhD, a professor of cell and tissue biology and of medicine, and a member of the Helen Diller Family Comprehensive Cancer Center at UCSF, showed that overexpression of a cancer gene called MYC (pronounced “mick”) in triple-negative breast cancer appears to drive tumors toward a dependency on fat metabolism to satisfy their appetite for a growth-fueling source of energy. The researchers succeeded in halting tumor growth with a drug, etomoxir, that targets fat oxidation. Etomoxir was originally developed to treat heart failure.
Goga previously led a study in which researchers determined that about nine out of 10 triple-negative breast cancers make excessive amounts of a protein encoded by the MYC gene, a well-known “oncogene” that drives the development of many tumor types. However, pharmaceutical companies have not been able to successfully target MYC despite decades of trying.
While early cancer-fighting strategies focused on rapid cell division in tumors, more recently scientists have increasingly been studying tumors’ abnormal metabolism. Goga and others previously discovered that MYC affects metabolic pathways as cancers develop.
High Rates of Glucose Metabolism in Tumors
Researchers have focused attention on abnormally high rates of glucose metabolism in tumors, first discovered nearly a century ago. However, for the new Nature Medicine study the scientists used a technique called mass spectrometry to identify metabolites associated with triple-negative breast tumors that arose in mice when MYC expression was abnormally elevated. In collaboration with the research group of Daniel K. Nomura, PhD, associate professor of chemistry and of nutritional sciences and toxicology at UC Berkeley, they found an unusual abundance of fatty acid oxidation metabolites, indicating that triple-negative breast cancer cells may be oxidizing fat to satisfy their energy needs.
In addition to studying these transgenic mice that had a switchable MYC gene, the researchers worked with human tumor tissue, with clinical data from The Cancer Genome Atlas (TCGA) and other public databases, and with tumor cells growing in the lab. UCSF graduate student Roman Camarda designed and conducted most of the experiments and wrote up the study for publication.
In triple-negative breast cancer cells with increased MYC activity grown in the lab, etomoxir inhibited production of the molecule ATP, the common energy currency of cells, but did not have the same effect on other types of breast cancer cells.
In an analysis of TCGA data from 771 breast cancer patients, the researchers found that 244 genes associated with fatty acid metabolism were expressed abnormally in triple-negative breast cancers, and they determined from their database analysis that abnormally controlled fatty acid oxidation is likely important for the sustenance of triple-negative breast cancers in humans.
ACC2 Enzyme and Survival Rates
From patient data, the researchers also determined that low levels of activation of the gene that makes the ACC2 enzyme, which normally restricts fatty acid oxidation, was associated with worse survival in breast cancer patients, especially those with triple-negative breast cancer.
The researchers transplanted human triple-negative breast tumor tissue into the mammary glands of mice, allowed the tumors to grow, and then injected the mice with etomoxir. Tumor growth was dramatically slowed by etomoxir treatment, and fewer metabolites associated with fat oxidation were produced. The treatment was not effective, however, in triple-negative tumors with low levels of MYC, indicating that high MYC expression combined with low levels of ACC2 may point to a subclass of triple-negative tumors that are vulnerable to inhibitors of fatty acid oxidation, the scientists concluded.
“This is very promising, but there is quite a bit more research to do before we can try this approach in humans,” Goga said. “Our goal is to try to identify fatty acid oxidation inhibitors and to ascertain which are likely to be most efficacious against these cancers, with the goal of bringing one to the clinic. It may be possible to repurpose drugs that already have been developed.”
Additional study authors include Shingo Kajimura, PhD, assistant professor of cell and tissue biology and a member of the UCSF Diabetes Center and the Eli and Edythe Broad Center of Regeneration Medicine and Stem Cell Research; and Alicia Zhou, PhD a postdoctoral fellow; Sanjeev Balakrishnan, a bioinformatics research specialist; Celine Mahieu, a master’s degree student; Brittany Anderton, PhD, a former graduate student; and Henok Eyob, PhD, a postdoctoral fellow, all in the Department of Cell and Tissue Biology at UCSF; Aaron Tward, MD, PhD, assistant professor of otolaryngology; Gregor Krings, MD, PhD, assistant professor of pathology; and Rebecca Kohnz, PhD, a post-doctoral fellow, in the Program in Metabolic Biology at UC Berkeley. Study funders included the National Institutes of Health, the Department of Defense Congressionally Directed Medical Research Programs, and the Atwater Foundation.
UC San Francisco (UCSF) is a leading university dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. It includes top-ranked graduate schools of dentistry, medicine, nursing and pharmacy; a graduate division with nationally renowned programs in basic, biomedical, translational and population sciences; and a preeminent biomedical research enterprise. It also includes UCSF Health, which comprises two top-ranked hospitals, UCSF Medical Center and UCSF Benioff Children’s Hospital San Francisco, and other partner and affiliated hospitals and healthcare providers throughout the Bay Area.