Martin McMahon
By Jeffrey Norris
Scientists are not in the business of making better mousetraps, but they're serious about making better mice to understand cancer biology.
Cancer sleuths are using new ways to genetically engineer mice. They use these new breeds of mice to study the effects of specific genetic alterations within tumor cells. With the new approach, genes that help trigger cancer are engineered into mice so that they can be turned on and off in specific organs at will. The mice offer what some researchers say is the most realistic animal model yet for studying human cancer.
Thanks to the latest techniques for genetically manipulating mouse embryonic stem cells, the cancers that arise in these new breeds of mice more faithfully recapitulate the development of cancer in human beings, says UCSF's Martin McMahon, PhD. Most important, tumor growth in these mice is driven by the same gene mutations that arise in human tumors, and in the same tissues.
McMahon and others are testing experimental drugs in the new mouse breeds and evaluating new molecular targets for future drug development. Depending on the combination of genetic abnormalities that enables each tumor to survive, grow and spread, researchers may ascertain the different drugs or drug combinations that work best for different tumors.
The older, established way to conduct preclinical testing of new cancer treatments on mice is to engraft human tumors under the skin of mice bred to lack a functioning immune system. "Although many experimental drugs can cure mice with such engrafted cancers, many of these drugs ended up failing in clinical trials," McMahon says. Such failures convinced cancer scientists of the need for better mouse models.
Probing Pathways in Skin, Lung and Thyroid Cancer
McMahon's lab team is using the new techniques to engineer and breed mice for studies of tumors that originate in the skin, lungs or thyroid. He has also distributed these mice to collaborators at UCSF and beyond who are studying colon, ovarian and prostate cancers and leukemia. McMahon's research with these recently bred mice already has begun to shed new light on the genetics of lung cancer.
McMahon is focusing on tumors in which cells are spurred to abnormal growth because of a mistake in the DNA blueprint for a protein called BRAF. The mutated gene encodes an unusually active form of the BRAF protein. In certain tissues and in a favorable environment, the altered protein made according to this blueprint pushes cells with the mutation to grow and divide with little restraint.
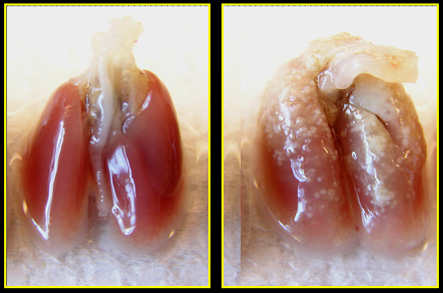 |
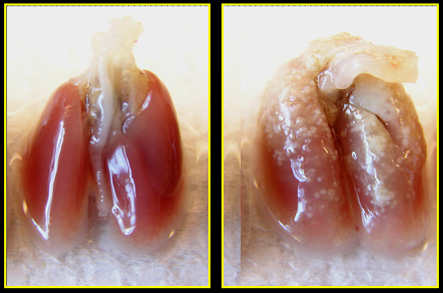
On the right, many early-stage tumors grow in the lungs of mice in which the protein BRAF is unusually active in cells. On the left, lung tumors do not grow profusely in similar mice that have normal BRAF. |
BRAF is one of several proteins that make up a particular biochemical relay team inside every cell. (See figure.) On this relay team, the baton is the growth signal these proteins pass as they run down this biochemical path - the MAP kinase signaling pathway, named after another protein on the signal-passing team. A genetic mutation in the gene that encodes BRAF can enhance the activity of the BRAF protein in this relay - similar to the way a steroid-enhanced training regimen can boost the performance of a sprinter.
BRAF itself is mutated and activated in many cancers - up to 70 percent of the deadly skin cancers known as melanomas, for instance. At least one member of this biochemical relay team appears to be unusually active in most cancers.
The new genetic engineering techniques make it possible to create mice that better mimic the effects of mutations that arise in BRAF - and in many other genes that are important in human cancers.
It took David Dankort, PhD, a postdoctoral fellow in McMahon's laboratory, nearly three years to breed mice and to complete recently reported experiments. The researchers discovered that multiple, early-stage lung tumors which arose in each mouse due to BRAF mutation stopped growing when treated with an experimental drug. The drug, PD0325901, made by Pfizer, blocks MEK, BRAF's partner on the signal-relaying team. The Pfizer drug now is being tested in human clinical trials.
Curiously, if left untreated, tumors in the mice that did not develop additional cancer-causing mutations also eventually stopped growing and became senescent. But when the researchers also inactivated the gene for a protective protein - the tumor suppressor known as p53 - untreated BRAF-induced tumors then progressed to become invasively growing lung cancers. Tumor suppressors, including p53, are inactivated in most invasive human cancers.
These results have strengthened McMahon's belief in the importance of finding ways to detect and treat tumors early, as well as of developing better therapeutics for later-stage disease, he says.
McMahon now is expanding his studies to include new breeds of mice with different cancer-inducing mutations. He is testing MEK inhibitors, as well as drug prototypes - developed by his UCSF collaborator, Kevan Shokat, PhD - that block other biochemical signaling pathways.
Related Links:
UCSF Comprehensive Cancer Center
McMahon Lab