Peripheral Vascular Disease: Keeping the Blood Flowing
By Steve Tokar
Rajabrata Sarkar, MD, PhD, describes his job as "taking care of people who have problems with poor blood flow to different parts of their bodies." In practice, it means that the San Francisco Veterans Affairs Medical Center vascular surgeon is constantly on his way to or from the operating room. He's happy to schedule time to discuss his work, as long as the questioner understands one proviso: "I may be in surgery."
Another likely place to find Sarkar, who is also a UCSF associate professor of surgery, is in the laboratory. There, he conducts basic research on causes of, and potential treatments for, peripheral vascular disease (PVD) - a narrowing or blockage of the arteries or veins outside the brain and heart - which affects about 10 million people in the United States.
Sarkar's research has a direct bearing on his clinical practice. Many of his patients suffer from inadequate blood flow in the legs - in particular, peripheral arterial disease (PAD) - which he says can result in "big trouble, and eventually lead to gangrene and amputation." But not for all patients: Some grow new arteries when the old artery is blocked. Others do not, though, "and those are the ones who get into trouble."
The problem, as Sarkar sees it, is that no one knows a reason for the difference. "We've come up with a lot of treatments for cleaning up, scraping out and bypassing arteries without really understanding why some patients have a poor response to PAD."
Much of Sarkar's research deals with matrix metalloproteinases (MMPs) - proteins that have shown promise in cell culture studies as agents for promoting arterial growth - and the genes that control their expression. Lately, Sarkar has been focused on the MMP-2 gene.
In a recent study, he and his research group mimicked PAD in the femoral (leg) arteries of normal, wild-type mice and in mice that lacked the MMP-2 gene. The wild-type mice grew new arteries. The transgenic mice did not; in fact, 40 percent lost a portion of a leg due to poor blood flow. Further experiments in mice revealed previously unknown and undescribed areas of the gene that are essential to its expression following injury.
"Clearly, the MMP-2 gene is very important to an animal's ability to grow new arteries in response to blockage," says Sarkar. His next step will be to study the same process in animal models of cigarette smoking, high cholesterol, diabetes and hypertension, which are the clinical conditions that most commonly cause vascular disease.
"Unfortunately, our patients often have at least two, and sometimes three or even four, of those conditions," he notes. "So one question is, do these conditions impair the expression of the MMP-2 gene? We think they do. Another is, is there less arterial growth as a result? We think there is. And then, can we identify the exact mechanisms by which MMP-2 expression is blocked under these conditions? If so, perhaps we could develop specific ways to increase arterial growth in patients with these problems."
Eventually, he says, MMP research may reveal a target for treatment. "Not in the next five or even 10 years - we're looking at distant horizons here - but if we don't understand the basics now, we're not going to come up with anything later."
Among American military personnel in Iraq and Afghanistan, there is another reason for damage to arteries: battle wounds, many of them caused by improvised explosive devices (IEDs). Sarkar explains that IEDs cause "a tremendous amount of damage to the arms and legs - shredded muscles and mangled limbs - and, of course, that damage involves arteries as well.
Military surgeons are very good at quickly repairing damage to major arteries, but we are seeing damage to arteries that are too small for surgical repair." Even if the limb is saved on the battlefield or in a military hospital, arterial damage will often cause long-term circulatory problems that can lead to later amputation.
To attack the problem, Sarkar has been funded by the Department of Defense to study gene therapy with various MMP genes as a potential key to battlefield wound treatment. "The eventual goal - and I'm talking many, many years from now - would be something that could be administered right there on the battlefield to repair arterial damage and kick-start new arterial growth, which would, of course, help injured civilians here at home too."
Vascular diseases are not restricted to arteries. More than 2 million Americans a year develop deep venous thrombosis, in which a blood clot develops in a vein, usually in the legs. With treatment, and sometimes spontaneously, clots can resolve, but "the process is poorly understood," says Sarkar. Clot resolution can lead to scarring and the destruction of the tiny valves within veins that keep blood moving in the right direction, which in turn can cause long-term problems such as swelling, pain and skin ulcers. This condition, known as post-phlebitic syndrome, disables more younger Americans than does arterial blockage.
"Again, differences among patients play a huge role," he says. "We see some folks after a large deep venous thrombosis and their leg is fine, whereas another patient with the same initial problem has a leg years later with nonhealing open ulcers, and they can't work or walk." Here again, the MMP genes appear to play a role; Sarkar is working to identify what that role might be and how various MMP genes might be used to accelerate healing of clots.
"In my work, the immediate satisfaction of seeing patients dramatically improve after surgery is often tempered by the suffering of other patients whose vascular problems are beyond the surgeon's reach," Sarkar concludes. "That's what motivates me in the laboratory: to understand the biology of these intricate processes, so that someday we can develop therapy for those we cannot help today."
Related Links:
New SF Neuroscience
Research Effort Will Help Troops, Veterans
UCSF News Release, December 7, 2005 Genetic Key to Growth of New Arteries Is Identified
UCSF News Release, November 30, 2005 San Francisco Veterans Affairs Medical Center advancing health worldwide™ website
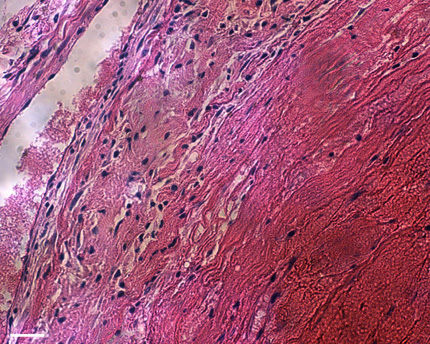 |
Photomicrograph of resolving deep venous thrombosis. |
 |
Angiogram of arterial regrowth in a mouse. Main artery to leg on left side has been removed and numerous small vessels have regrown to supply the leg. |
UCSF News Release, December 7, 2005 Genetic Key to Growth of New Arteries Is Identified
UCSF News Release, November 30, 2005 San Francisco Veterans Affairs Medical Center advancing health worldwide™ website