End-of-Life Expert Comments on Physician-Assisted Suicide Ruling

The US Supreme Court's decision on Jan. 17 to uphold Oregon's assisted-suicide law leaves intact state control over whether physicians can help people with a terminal illness end their lives. The decision was a defeat for the Bush administration, which the high court ruled had exceeded its authority in trying to undo Oregon's voter-approved statute by punishing doctors who help terminally ill people die. The ruling allows the state of Oregon - the only state in which physician-assisted suicide is legal -- to continue to follow the law. "It could also portend agonizing debates elsewhere in the United States, as medicine advances and people continue to wrestle with questions of life and death," reported the New York Times. Steven Pantilat, MD, a national expert on palliative and end-of-life care and director of the Palliative Care Service at UCSF, says most patients who ask for assisted suicide decide not to pursue it once their pain, depression and other issues are appropriately addressed. Launched in 1999, the UCSF Medical Center Palliative Care Service focuses on helping patients achieve the best possible quality of life. The service includes physicians, nurses, chaplains, social workers and pharmacists who work together to address many of the issues that arise for patients facing the end of life and for their families, according to Pantilat, associate professor of medicine and Alan M. Kates and John M. Burnard Endowed Chair in Palliative Care. In April 2004, UCSF was named one of six leadership centers in the country for training health care professionals who want to start palliative care programs. While interest in end-of-life care is growing, only 22 percent of hospitals in California offer these services to patients, according to Pantilat.
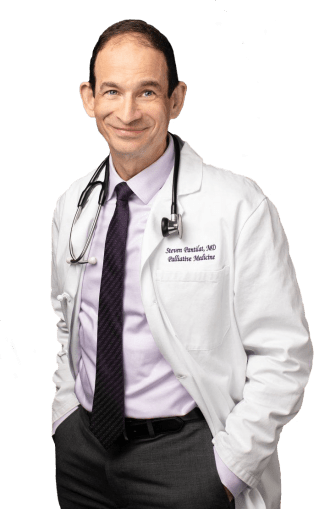
Pantilat answered the following questions about the recent Supreme Court ruling.
Do you think other states now will follow Oregon's lead and pursue laws allowing physician-assisted suicide?
This ruling will let other states know that if they pass such laws, they will be upheld. However, I don't see a flood of similar laws in the wake of this decision. My hope is that this ruling will shine a light on the generally poor quality of care available to many people facing the end of life, and promote palliative care programs to address unmet needs for patients facing the end of life.
Do you think the federal government should override state law on standards for care and treatment, including end-of-life issues?
Absolutely not. These decisions are best left between physicians and their patients. Any regulation on the patient-doctor relationship is best done at a state level to most closely reflect the attitudes and practice within the community.
As baby boomers age, do you think physician-assisted suicide will become more widely accepted and practiced?
The Oregon experience shows that this approach can work without abuses. Over time, this will likely be more accepted. What is more important, however, is that all people have access to high-quality palliative care as they face the end of life so that they can receive expert pain and symptom control and attention to other important issues. Most people who ask for assisted suicide decide not to pursue it once their pain, depression and other issues are appropriately addressed. It is only a very small minority of patients who make use of assisted suicide. This is why it is so important that patients have the full range of options and access to high-quality palliative care such as we provide here at UCSF through the Palliative Care Service and the symptom management program at the UCSF Comprehensive Cancer Center at Mount Zion. Source: Lisa Cisneros Links: UCSF Palliative Care Service