A protein that contributes to the rejection of transplanted hearts has been identified by a UCSF research team. The finding raises hopes for future developments that may boost transplant success and reduce the side effects of current anti-rejection drugs.
The protein - called NKG2D - might also play a role in the rejection of other organs, say transplant surgeon Sang-Mo Kang, MD, and immunologist Lewis Lanier, PhD.
The UCSF researchers found that regularly injecting mice with antibodies targeted against NKG2D can help prevent heart transplant rejection.
Further research might lead to human studies of drugs that block these same proteins - and to new drug cocktails that cause the immune system to better accept transplanted organs.
 |
Sang-Mo Kang |
"There's a good chance it could be applicable in humans," says Kang.
Transplant recipients face lifelong use of drugs that prevent the immune system from rejecting their transplants. But the drugs also suppress beneficial immune responses. That is why transplant recipients are especially susceptible to infection. The drugs have other harmful side effects - they may cause kidney damage, for instance. Clinicians have long wished for better anti-rejection drugs.
At a minimum, the UCSF researchers have glimpsed the molecular essence of a long-frustrating and still mysterious phenomenon. The studies set the stage for additional research that will further deepen scientific understanding of transplant rejection.
Curiosity Leads to Collaboration Across Disciplines
The collaboration began after Kang heard Lanier give a talk on his research as part of a weekend-long retreat for UCSF and UC Berkeley immunologists. The two discussed whether surgery might cause stressed cells near the surgery site to undergo an immune response like the one Lanier described during his talk. They decided to investigate.
 |
Lewis Lanier |
The mice in the experiments ended up with two hearts. Postdoctoral associate Feng-Chun Liu did most of the mouse heart transplants, hooking up the donor aorta and pulmonary vein to the recipient's aorta and vena cava, respectively. Liu performed his surgery while viewing the surgical field under an operating microscope, sewing up vessels as thin as fine spaghetti.
The transplanted hearts do not pump blood, but they do beat normally. The beating of the transplanted hearts provides a good way to keep an eye on transplant function. The researchers compared transplants between genetically identical and genetically distinct mice. They evaluated heart function, rejection and immune responses, and tracked key molecules.
Natural Killers
The NK in NKG2D stands for natural killer. Natural killer cells are among the early responding cells of the immune system. They were first appreciated for their anticancer properties. Lanier is an international expert on natural killers. Together with Thomas Spies' research group at the Fred Hutchinson Cancer Research Center in Seattle, Lanier identified a role for NKG2D in the activation of natural killer cells and T cells in the immune response against tumors and virus-infected cells.
Kang and Lanier have now demonstrated that natural killer cells and T cells that make and exhibit NKG2D on their cell surfaces also appear to play a role in transplant rejection. The NKG2D molecules bind to proteins displayed on the surfaces of tumor cells and virus-infected cells. This connection allows the immune cells to become activated and to attack these abnormal cells.
Lanier's lab group first identified the mouse version of the proteins - named RAE-1 proteins - that are recognized by NKG2D. The human versions have also been identified. In both mice and humans, these NKG2D-binding proteins are absent in most healthy cells most of the time.
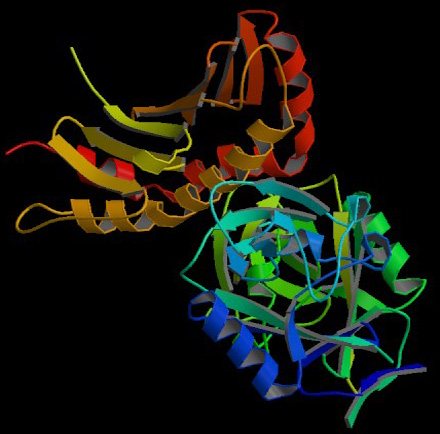
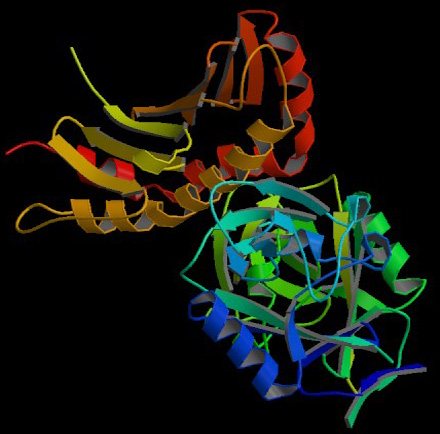 |
PDB ID: 1JSK.
Li, P., McDermott, G., Strong, R.K.
Crystal structures of RAE1-beta and its complexd with the activating immunoreceptor NKG2D.
Immunity 16:77-86 (2002)
|
Lanier has concluded that RAE-1 proteins are switched on by cells to signal that they are stressed or damaged. These NKG2D-triggering proteins are turned on during many viral infections, for instance.
"Switching on RAE-1 proteins is one way for cells to say they are unhappy," Lanier says. Immune cells, including natural killer cells and T cells, home in on the nonperforming, discontented cells and target them for destruction. Kang and Lanier wanted to see whether cells in a transplanted organ would make RAE-1 proteins and help trigger immune rejection in response to transplant surgery.
Preventing Transplant Rejection
The stress of transplant surgery proved sufficient to cause the transplanted tissues to make RAE-1 proteins. RAE-1 production peaked three days after surgery. Mice made RAE-1 even when they received hearts from genetically identical mice - transplants which are not rejected.
But mice that received genetically foreign hearts also had a second and ongoing surge of RAE-1 production a few days after the first peak. The foreign transplanted hearts stopped pumping as rejection set in. NKG2D-expressing CD8+ T cells of the adaptive immune response were clearly implicated in this transplant rejection response.
The researchers did not observe the second wave of RAE-1 production in hearts transplanted from genetically identical mice.
To prevent rejection of the genetically foreign hearts, the researchers used an antibody that blocks the NKG2D protein on the natural killer cells and T cells, and combined it with a second, commercially available drug named CTLA4-Ig. CTLA4-Ig already is in use in humans for the treatment of autoimmunity.
UCSF surgical resident Jim Kim, who helped to carry out the experiments, presented the team's preliminary findings at the World Transplant Congress this past July.
Related Links:
Lanier Lab