30 Years On, Are We Winning the Fight Against Alzheimer’s?
Lecanemab, Donanemab, Drug-Free Strategies Emerge as New Weapons Against Dementia
UC San Francisco experts say that we have reached a pivotal point in Alzheimer’s disease research, 30 years after the first pharmaceutical came to market. On Jan. 6, 2023, the Food and Drug Administration is expected to give accelerated approval of lecanemab – one of the first drugs to attract widespread enthusiasm among neurologists, after showing positive phase 3 results in slowing the progression of early-stage disease.
The UCSF-tested drug is a monoclonal antibody, a lab-made protein, that targets amyloid plaques that accumulate between neurons and disrupt cell function, setting off a cascade of events that ultimately lead to memory loss.
We asked UCSF experts from the Memory and Aging Center, the UCSF Weill Institute for Neurosciences and the Alzheimer’s Disease Neuroimaging Initiative to share their insights on Alzheimer’s therapies on the horizon, some of which may be effective even before symptoms emerge, as well as drug-free interventions that may prevent or slow the disease.
Which Alzheimer’s drugs, currently in development, are you most optimistic about?
Kristine Yaffe, MD: I’d say lecanemab and donanemab, the latter of which has demonstrated a significant clearance of amyloid plaque after six months of treatment for 38% of clinical trial participants. Both lecanemab and donanemab trials studied patients with mild cognitive impairment and early-stage Alzheimer’s disease, and have the best evidence of benefit and a better side effect profile than Aduhelm. Aduhelm was the first anti-amyloid therapy. It’s currently available only in trials, after Medicare noted concerns about safety and efficacy.
Michael Weiner, MD: Agree that lecanemab and donanemab are promising. On average, lecanemab patients experienced a 27% slowing of the rate of progression compared to placebo, with some patients showing a better treatment response than others. We do not have enough information at this time to identify which patients are more likely to benefit.
Yaffe: We should keep in mind, though, that while 27% sounds big, it all depends on 27% of what. If it’s 27% of a modest decline, that’s very small, whereas 27% of a big decline is significant. It will be difficult to know if the impact is clinically significant until more studies are conducted.
How safe are these new drugs?
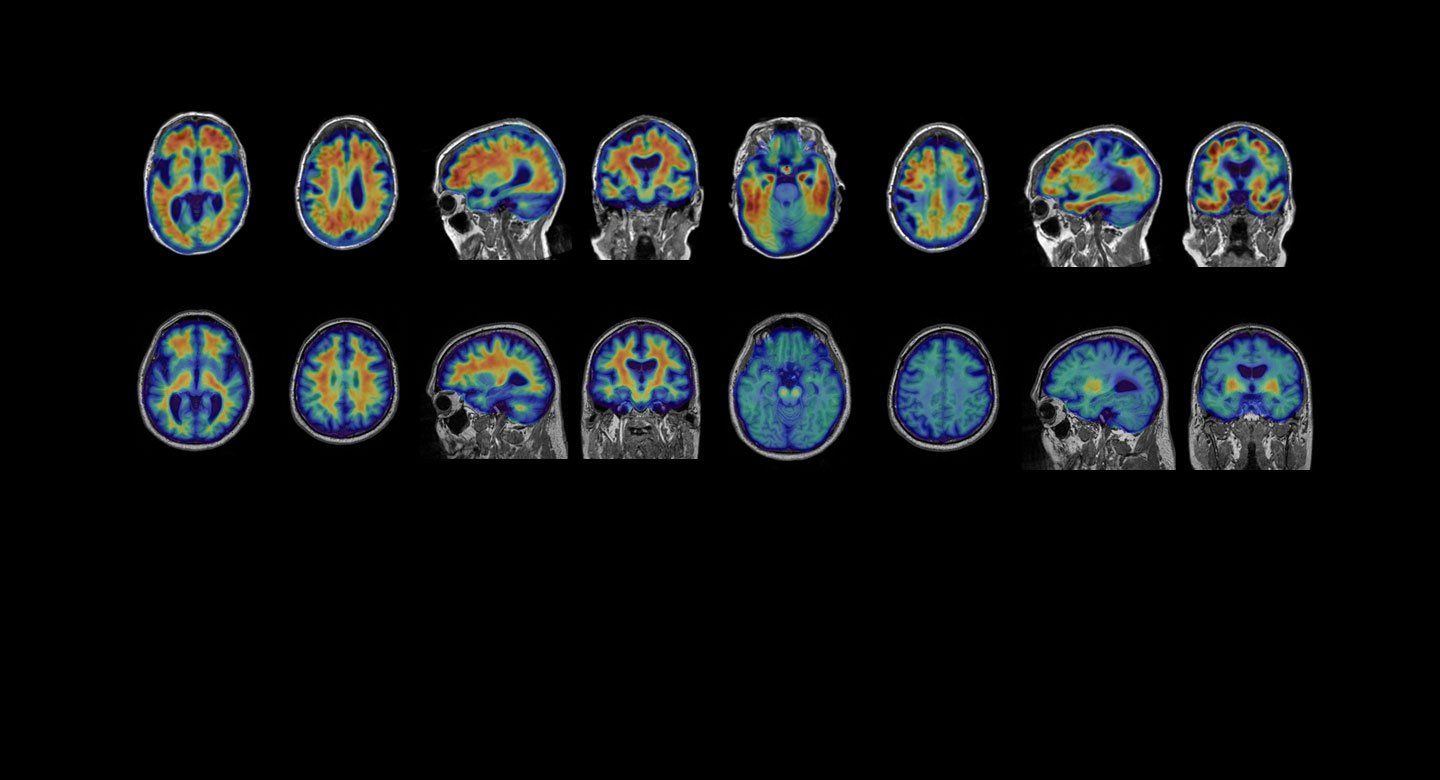
Gil Rabinovici, MD: One potentially serious adverse effect is amyloid-related imaging abnormalities (ARIA), which occur in patients treated with anti-amyloid therapies. This refers to swelling or microscopic bleeds in the brain. ARIA will need to be monitored closely with serial MRI, especially as patients initiate treatment. However, in the lecanemab trial, it was asymptomatic in 80% and very rarely associated with serious symptoms. The swelling typically resolves spontaneously and most patients can resume treatment. A genetic test will likely be recommended, since some variants of APOE, a gene that increases the risk of Alzheimer’s, are associated with a higher risk of ARIA.
Are researchers developing drugs for patients whose disease has progressed beyond the mild stage?
Adam Boxer, MD, PhD: There are a variety of treatments in development for later stage Alzheimer’s patients, such as sigma2, growth factor receptor modulators and some tau-targeting therapies, but none have yet demonstrated convincing clinical evidence of efficacy.
Rabinovici: As a field, we’re striving to develop therapies for all stages of the disease. However, based on our understanding of the biology, we believe that anti-amyloid therapies may be the most useful in early disease stages, and that’s where they’re being tested. Current data indicates it wouldn’t be appropriate to use lecanemab for patients with moderate to severe Alzheimer’s. Later stages of Alzheimer’s will likely require other drug targets and therapeutic approaches.
Have any drug trials demonstrated a reversal in cognitive decline?
Weiner: There is some research aimed at stimulating neuron growth, which, if successful, would have the potential to increase cognition. So far, the early results have been very limited. We’re a long, long way from restoring cognitive function in people with dementia or mild cognitive impairment.
The costs of anti-amyloid therapies are expected to cost tens of thousands of dollars. If lecanemab and donanemab are approved, would you expect Medicare to cover costs?
Rabinovici: Medicare announced in April 2022 that anti-amyloid therapies, as a class, would only be covered in research studies, but this decision was based on Aduhelm’s ambiguous phase 3 data. It’s increasingly apparent that each antibody should be judged separately as they are biologically distinct. My hope is that lecanemab will be granted full approval, based on clinical efficacy, and that Medicare and other payers will cover appropriate patients. The timeline isn’t clear. In my opinion it may take a year or longer to sort out coverage.
Some experts suggest that 30% or more of Alzheimer’s might be attributed to modifiable risks like smoking, obesity and low cognitive stimulation. How does risk-reduction compare to medication in treating Alzheimer’s?
Yaffe: It’s hard to compare apples to oranges. Risk-reduction strategies tend to be more for primary prevention in non-cognitively impaired older adults who may or may not be at risk. Most of the latest amyloid antibody trials are for people with mild cognitive impairment or early Alzheimer’s. Some risk-reduction trials have shown better cognition over time, but others have not shown benefit. Since these strategies are low cost, low risk and benefit heart and overall health, we probably want to offer them to older adults and possibly even in midlife.
Boxer: A big topic of discussion lately is how we might combine treatment approaches in future clinical trials to look for additive or potentially synergistic effects. It will be exciting to test how combinations of risk-reduction strategies and disease modifying therapies might lead to larger benefits.
Weiner: Many of these strategies require high compliance and not everyone is able or willing to take on such changes. The benefits of healthy eating and exercise are very well known, yet a substantial fraction of the public ignores these instructions. But people would be willing to take a pill for Alzheimer’s, just like they take a pill for hypertension or high cholesterol.
Yaffe: My hope is that Alzheimer’s disease will be treated like cardiovascular disease with several drugs – one for amyloid, tau, maybe inflammation – together with risk-reduction strategies.
Actor Chris Hemsworth revealed he found out at age 39 that he has two copies of the APOE4 gene variant, putting him at increased risk for Alzheimer’s. Do you recommend finding out about your risk, either by physician-ordered blood biomarker tests and scans, or by the straight-to-consumer DNA product 23andMe?
Rabinovici: Expert guidelines currently do not recommend that asymptomatic people undergo genetic or biomarker testing to evaluate their risk of Alzheimer’s outside of research studies. This view is likely to change, especially if therapies are approved that delay or prevent the onset of symptoms.
Boxer: I agree. This is a rapidly evolving field and I expect there will be changes in practice over the next few years. We are excited about the potential of blood biomarker tests to improve access to care and clinical trials in underserved populations.
Rabinovici: I personally do not recommend straight-to-consumer genetic testing for APOE4. Interpreting the results is not straightforward, and results may have implications for first-degree family members who may prefer not to know about their risk. Before pursuing any testing, I recommend discussing with an Alzheimer’s specialist or genetic counselor.
Weiner: Some studies now inform participants of their biomarker results, including the Alzheimer’s Disease Neuroimaging Initiative. With genetic testing and blood-based biomarkers for Alzheimer’s becoming available for the public outside of a clinical setting, clinicians need to be prepared to help patients understand their meaning in the context of their lives.
My hope is that Alzheimer’s disease will be treated like cardiovascular disease with several drugs – one for amyloid, tau, maybe inflammation – together with risk-reduction strategies.
Kristine Yaffe, MD