Will Cell Therapy Become a 'Third Pillar' of Medicine?
Treating patients with cells may one day become as common as it is now to treat the sick with drugs made from engineered proteins, antibodies or smaller chemicals, according to UC San Francisco researchers who have outlined their vision of cell-based therapeutics as a “third pillar of medicine.”
Wendell Lim, PhD
“Today, biomedical science sits on the cusp of a revolution: the use of human and microbial cells as therapeutic entities,” said Wendell Lim, PhD, a UCSF professor and director of the UCSF Center for Systems and Synthetic Biology, and one of the co-authors of an article published online April 3 in Science Translational Medicine.
Cell therapies have the potential to address critical, unmet needs in the treatment of some of the deadliest diseases, including diabetes, cancer and inflammatory bowel diseases, the scientists said.
The reason, they said, is that cells can carry out functions that can’t be performed by small-molecule drugs produced by Big Pharma, or by targeted drugs developed by biotech firms in the wake of the genetic engineering revolution. For one, cells are adaptable. They can sense their surroundings better than today’s drugs and can vary their responses to better suit physiologic conditions.
Continued advances in cellular engineering could provide a framework, according to the co-authors, for the development of cellular therapies that are safe and that act predictably.
Joining Lim as co-authors of the Science Translational Medicine article are Michael Fischbach, PhD, assistant professor in the UCSF School of Pharmacy and an expert on the human microbiome, and Jeffrey Bluestone, PhD, executive vice chancellor and provost at UCSF and a leading diabetes and transplant rejection researcher.
The three also have organized a daylong symposium on the potential of cell therapy on April 12 supported by UCSF and the journal Science Translational Medicine, featuring talks and discussion by some of the nation’s leading scientists in stem cell therapy, immunotherapy and the human microbiome – the latter consisting primarily of the many hundreds of interacting species of bacteria that live within and upon us.
Advances in Cell Therapies
It has been more than four decades since cells were first used successfully in bone marrow and organ transplants, but the strategies envisioned today are more complex, involving manipulating cells based on new knowledge of how genes program their development and inner workings.
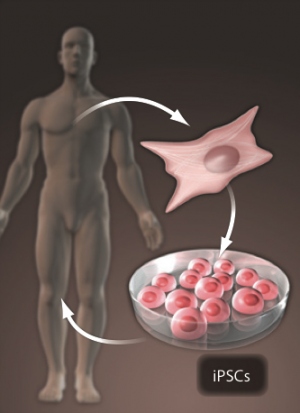
For some medical applications, cell therapies are better
equipped than small-molecule or genetically-engineered drugs.
For instance, individually tailored, induced pluripotent stem
cells might be used to regenerate damaged organs or tissues.
Graphic courtesy of Science Translational Medicine
Cells of the immune system are among those that naturally carry out critical functions, but researchers are working on manipulating them to create better-targeted and more effective therapies. For instance, immune responses directed against cancer often are weak, so scientists are engineering and growing populations of immune cells that target specific molecules found on cancer cells. Already, remarkable recoveries from deadly leukemia have been credited to these new experimental treatments.
Bacterial cells also are showing promise for therapy. In recent years, scientists have come to appreciate that 90 percent of the cells living within and on our bodies are bacteria and that these microbes interact with our own cells and affect our health.
The potential of bacteria to treat disease has been demonstrated dramatically by the recent use of fecal transplants to introduce communities of health-promoting bacteria into patients with recurrent Clostridium difficile infections, a serious gastrointestinal condition that can be life-threatening. Combinations of bacteria that also are engineered to fight inflammation might prove to be even more effective in treating Crohn’s disease and other inflammatory bowel diseases, according to the UCSF scientists.
Other “killer apps” for cell therapies might include combinations of bacterial and human engineered cells. For instance, to control weight gain, gut bacteria might be deployed to convert certain carbohydrates into non-digestible forms, and also to signal engineered human cells lining the epithelial walls to trigger a program that sends a message to the brain that appetite has been satisfied.
Still, many engineering and regulatory challenges to cell therapy remain, the authors concede.
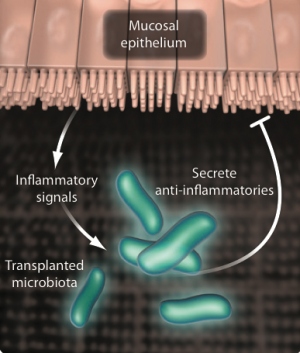
In this example of the advantages of cell therapies, bacteria
may be programmed to make an anti-inflammatory molecule
and transplanted to the gut to treat inflammatory bowel disease.
Graphic courtesy of Science Translational Medicine
Scientists want to be able to reliably control many aspects of cells, including their activation, population growth, programmed death, migration to specific sites in the body, interactions and communications with other cells, production of small therapeutic molecules, and decision making.
While the complexity of cells makes many scientists leery of cell therapies, the authors said, this complexity might make cell therapies more predictable than other drugs, because complicated, naturally occurring feedback circuits tend to restrict cellular activity. Just as cells already use molecular circuits to act very precisely, researchers ought to be able develop a systematic understanding of the cell’s control modules to tune and reshape how cells behave.
“If small molecules and biologics are tools, then cells are carpenters — and architects and engineers as well,” Fischbach said.