William L. Holzemer
For a number of years, the UCSF School of Nursing has been leading the way in examining the impact of stigma as it relates to nurses who care for HIV patients in developing countries.
Sociologists define stigma as “a powerful discrediting and tainting social label that radically changes the way individuals view themselves and are viewed as persons.”
“We are learning that HIV stigma impacts people’s decision to get HIV-tested, decisions to disclose their HIV status, adherence to HIV medications and their day-to-day quality of life,” said William L. Holzemer, RN, PhD, professor and associate dean of international programs and Lillian and Dudley Aldous Endowed Chair in Nursing Science in the School of Nursing. “HIV stigma also impacts the quality of work life for nurses, as they are perceived by some to be contagious, since they work with HIV-positive patients.”
Findings from a recent study were published in the
Journal of Advanced Nursing in a paper, titled “A Conceptual Model of HIV/AIDS Stigma from Five African Countries.” The study examined the dynamic nature of stigma as reported by study participants, which included persons living with HIV and nurses. The research is supported by a grant from the Fogarty International Center of the National Institutes of Health.
The study looked at developing culturally appropriate measures of stigma, as perceived by people with HIV/AIDS and by nurses, to test how stigma is related to the quality of care and quality of work life. The study also sought to pilot-test a stigma reduction intervention strategy.
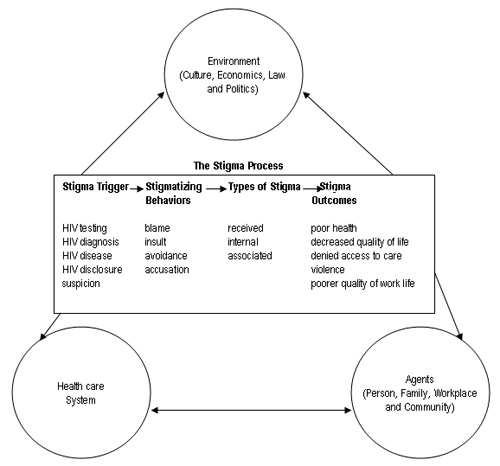
Research showed that the stigma process includes four dimensions: triggers of stigma, stigmatizing behaviors, types of stigma and the outcomes of stigma. The conceptual model below shows the dynamic nature of stigma. According to researchers, the model may be used to identify areas appropriate for the design and testing of stigma reduction interventions.
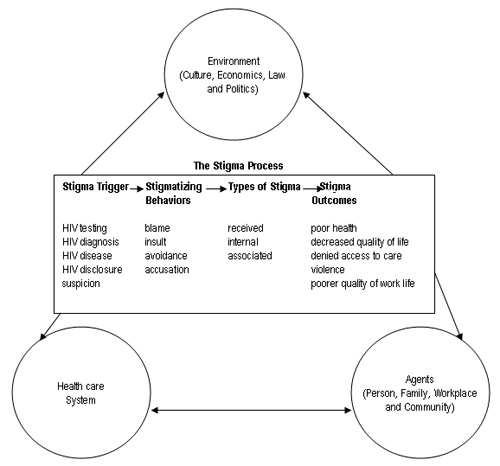
Chart by William L. Holzemer, Leana Uys, Lucy Makoae, Anita Stewart, René Phetlhu, Priscilla S. Dlamini, Minrie Greeff, Thecla W. Kohi, Maureen Chirwa, Yvette Cuca and Joanne Naidoo.
“This model helps us to understand what triggers HIV stigma,” said Holzemer. “When an HIV-positive person starts taking HIV medication treatment, it is sometimes assumed they must be perceiving less HIV stigma. This model suggests that going on treatment may actually serve as a trigger to being the recipient of more HIV stigma.”
The idea is that, with this new information, nurses can counsel patients about the potential for experiencing new types of HIV stigma when a patient begins taking antiretroviral therapies. This, in turn, will help the patient be better prepared to take the medications as prescribed.

Raymond Phillips takes a break in UCSF's Saunders Court.
Photo by Shipra Shukla
Many of the lessons learned in Africa can be applied to other developing countries. Raymond E. Phillips, RN, retired commander of the US Navy Nurse Corps and a fourth-year doctoral candidate in the UCSF School of Nursing, recently returned from Chennai, India, as a fellow of the Fogarty International Clinical Research Scholars Program. While there, Phillips conducted research for his dissertation, a descriptive, correlational study exploring the impact of HIV and AIDS-related stigma on hospital-based nursing care.
“While both Africa and India experience resource shortages, the density of people in India — it has the second-largest population in the world — and how nurses are thought of culturally add another layer of difficulty,” said Phillips. “The status of nurses is quite low, and added stigma has an impact on their self-esteem and often how they care for an HIV patient.”
Phillips was the first nurse to receive a Fogarty Fellowship. His time in Chennai centered around a partnership with the Y.R. Gaitonde Center for AIDS Research and Education (YRG CARE). Founded in 1993, YRG CARE partners with the World Health Organization to lead the fight against HIV/AIDS in India.
Phillips commented on the lack of resources at government hospitals in India and the contrast it posed against India’s burgeoning, new economy, which seemed superficially removed in a country faced with a rising AIDS pandemic.
“The sheer volume of patients at the government hospital in Chennai was overwhelming,” said Phillips. “There were often 15,000 patients coming through in one day — many of them with HIV — and there would only be 10 nurses and even fewer doctors to treat all of them. All this among neighborhoods with fancy hotels, limos and new American-style shopping malls.”
Stigma often forces those who have HIV to receive care at these government hospitals, since health care providers at private hospitals can refuse to offer care. Due to the lack of opportunity to improve their skills, which can in part be attributed to the need to focus on the volume of patients, as well as the lack of an institutional review board, many nurses in India do not have the adequate knowledge and skills needed for treating HIV/AIDS patients and conducting research. As a result, they consistently request additional basic education in that area.
While in India, Phillips addressed this need by teaching a number of courses and collaborating with the International Training and Education Center on HIV (I-TECH), a project of UCSF, the University of Washington and the Indian government, to assist in providing the nurses at YRG CARE with opportunities for continuing education.
Phillips’ time spent teaching courses to nurses in India and fostering discussion about the status of the profession is an example of how UCSF seeks to build capacity in the developing world. In sharing the lessons learned with partners in India and Africa, UCSF trainees and researchers are addressing health disparities that impact the world’s most vulnerable populations.
“Nurses are basically trained as helpers to physicians in a governing system that systematically subjugates nursing to medicine,” said Phillips. “While the status of nursing as an independent science has been established in the United States, it is a dream yet to be realized in India.”
A Conceptual Model of HIV/AIDS Stigma from Five African Countries
Journal of Advanced Nursing (June 2007) 58(6):541-551
William L. Holzemer, Leana Uys, Lucy Makoae, Anita Stewart,
René Phetlhu, Priscilla S. Dlamini, Minrie Greeff, Thecla W. Kohi,
Maureen Chirwa, Yvette Cuca and Joanne Naidoo
Abstract | Full Text
Related Links:
Changing the Face of Nursing